The first is considered the most accurate indicator of the content of mineral salts in bone tissue.
The second is no less important, since its correlation with the risk of fractures is very high, so this index has great prognostic value. Interpretation of densitometry results may also contain one more parameter - volumetric mineral density of tissues, but it is used less and less. This is due to the fact that it is quite difficult to detect and often in order to obtain such a parameter it is necessary to use a special type of computed tomography and use quite expensive methods of data processing.
How to prepare for densitometry?
A bone study such as densitometry involves examining the distal part of the bone tissue, and then the epiphyses of the bones. To get the most reliable results, the patient must:
- one day before the diagnosis, refuse any calcium-containing food supplements and medications;
- notify the doctor about any procedures using contrast - densitometry cannot be performed for some time after them;
- do not move during the procedure and do not change the position of the body and limbs.
Now you know how to prepare for densitometry, and it becomes clear that no special preliminary procedures will be required.
Types of densitometry - why is bone density testing performed?
The diagnostic method under consideration comes in several types:
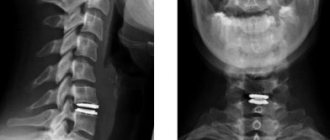
- X-ray . Two types of X-rays are used to study the structure of bone tissue. By comparing information on the absorption of emitted energy, the doctor assesses the level of deviation from the norm in bone density. This manipulation takes a minimum of time, and the radiation dose is 400 times less than with standard radiography. This type of densitometry is used when it is necessary to study the bone tissue of the hip joint, shoulder, forearm, lumbosacral spine, or the entire spinal column.
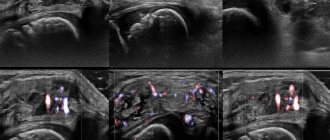
- Ultrasonic. Due to the absence of any radiation exposure, this technique is considered absolutely safe. It can be used on children as well as pregnant women. However, the effectiveness of this manipulation is lower than that of x-ray densitometry. Its principle is based on calculating the speed at which ultrasound waves propagate through bone structures. Bone density is directly proportional to the rate of absorption of rays by bone tissue. If there is significant loss of bone mass, X-ray densitometry is prescribed. With its help, it is possible to obtain information about the elasticity, strength of the cortical layer, as well as the thickness of individual microstructures.
- Quantitative computed tomography . Makes it possible to obtain a three-dimensional picture of the structural density of bone elements. Since the radiation load with this technique is very significant, it is used very rarely in practice.
Due to a decrease in calcium levels in the bones, the diagnostic method in question is prescribed to people after they reach 50 years of age. It is at this age that there is a high probability of osteoporosis , which, according to statistics, ranks third in mortality.
The following categories of people need to measure the value of mineral density of bone structures:
For those who have two or more phenomena that provoke osteoporosis:
- Women who experienced menopause at an early age (before 45 years).
- Pronounced thinness.
- Presence of osteoporosis in close relatives.
- Deficiency of calcium and/or vitamin D in the daily diet.
- Sedentary lifestyle.
- Tobacco smoking.
- Hormonal imbalances.
- Alcohol abuse.
- Treatment with corticosteroids.
Diabetes.
Serious problems with the kidneys.
A history of rheumatic pathologies: systemic lupus erythematosus, vasculitis, scleroderma, etc.
Frequent bone fractures, which can occur even with minor trauma.
Various pathologies of the spine.
The diagnostic procedure in question is not performed in the following cases:
- Gestation period (for X-ray densitometry).
- Deformations in the lumbosacral section of the spine, which prevent the patient from adopting the correct body position during the examination.
- Carrying out diagnostics using barium contrast less than a week before the specified manipulation.
Types of research
There are two types of such procedures: X-ray and ultrasound. Each of these methods is more effective when examining certain parts of the body. For example, ultrasound is used to determine problems in the heel bone, as it provides more information, and the x-ray method is advisable to use when it is necessary to examine the femoral neck or lumbar spine
.
X-ray densitometry
If you have been prescribed such a procedure, it is worth finding out what densitometry is and how it is performed in order to understand what to be prepared for. This method is more informative, but it is also less gentle. You can undergo the study no more than once a year, but this may not be enough. However, the radiation dose will be small - much less than with a standard x-ray. This procedure will allow you to identify even minimal deviations in bone tissue and accurately determine its density based on exactly how the rays will pass through the bones. This method is also very informative when examining the wrists.
Ultrasound densitometry
If you do not know how bone densitometry is done using ultrasound, you should know that it is the safest and has no contraindications. It is even prescribed to pregnant and lactating women. This procedure is carried out using a special densitometer, the operation of which is based on the passage of ultrasound through the patient’s bones. The advantage is that such diagnostics can be carried out both to identify and control the disease as often as desired.
First experience of using anidulafungin in the treatment of patients with candidemia
Wedge. and experiment. hir. Journal them. acad. B.V. Petrovsky. - 2013. - No. 2. - P. 41-46.
Infections caused by microscopic fungi represent a serious problem in modern hospitals, especially in critically ill patients receiving repeated courses of antibiotics, as well as in intensive care unit patients. According to the SCOPE study, fungi of the genus Candida
occupy 4th place among the causative agents of nosocomial infections in the United States, second only to coagulase-negative staphylococci, Staphylococcus aureus and enterococci [1].
If until recently systemic fungal infections were mainly the lot of immunocompromised patients (cancer patients, patients on immunosuppression, etc.), now they are much more often recorded in complicated medical and surgical patients. The introduction into clinical practice of new high-tech treatment methods that support the lives of critically ill patients has led to an expansion of indications and an increase in the volume of surgical interventions performed. Improvements in intensive care techniques have significantly increased the life expectancy of critically ill patients, leading to an increase in the proportion of patients with risk factors for developing fungal infections.
According to various authors, the mortality rate for invasive candidiasis reaches 30-50%, which in some cases is significantly higher than for infectious complications of bacterial etiology [2, 3].
Currently, about 200 species of fungi of the genus Candida
that can cause infectious diseases in humans. These opportunistic microorganisms are unicellular eukaryotes, which, compared to bacteria, have a higher level of cellular organization. The presence of chitin in the cell wall and its relatively large size (5-12 microns) make it difficult to inactivate fungal cells by factors of the body’s immune system, and the production of various enzymes (proteolytic, lipolytic, carbohydrase), which are factors of aggression and permeability, promotes the penetration of fungi into epithelial cells and distribution in tissues.
Fungi of the species Candida albicans
are representatives of normal intestinal microflora.
However, this species is the most common causative agent of candidiasis in all countries of the world. However, in recent years there has been a clear trend towards an increase in the proportion of infections caused by non- albicans
Candida species, especially
C. parapsilosis
,
C. glabrata
and
C. tropicalis
[1]. There is also a decrease in the sensitivity of candida to the basic antifungal drug, fluconazole, which makes traditional therapy highly likely to fail [4].
Unlike antibiotics, the arsenal of antifungal drugs is relatively small. The structural and biochemical similarity of fungal cells with the cells of a macroorganism makes it difficult to find drugs that have both high antifungal activity and low toxicity. Thus, many antifungal drugs act on enzyme systems, disrupting the synthesis of steroid hormones and prostaglandins in the body.
A number of antimycotics are inappropriate for use in systemic fungal infections. Thus, the polyene drug nystatin is not absorbed when taken orally, so it is used exclusively to reduce fungal colonization or treat superficial candidiasis of the mucous membranes of the gastrointestinal tract. The imidazole derivative ketoconazole in therapeutic concentrations acts as a fungistatic, which creates a high likelihood of relapse. In addition, the drug has a fairly high toxicity and is used only orally. Itraconazole is of great value for systemic mycoses, since it is less toxic and in much lower concentrations than ketoconazole, it acts on the enzyme systems of fungal cells, suppressing the synthesis of ergosterol. However, itraconazole has a negative inotropic effect, reducing cardiac output, so its use in patients with severe diseases of the cardiovascular system is undesirable.
The use of amphotericin B is limited by the high toxicity of this drug, and in many cases it is impossible to use doses that create effective tissue concentrations in severely ill patients. The liposomal form of amphotericin B has significantly less toxicity. However, to date liposomal amphotericin B has not been registered and is not supplied to the Russian Federation.
The first-line drug for the treatment of candidiasis over the past two decades has been fluconazole. Due to its good pharmacokinetic properties, it is highly effective not only when administered parenterally, but also when administered orally. However, as noted above, recently, according to various studies, there has been an alarming trend of increasing resistance of fungi of the genus Candida
to fluconazole.
This is explained both by the unreasonably widespread use of drugs from the azole group and by the increasing frequency of infections caused by Candida
non-
albicans
with reduced sensitivity to fluconazole [1]. It is important to consider that Candida strains isolated in the ICU are significantly more likely to have an unfavorable antifungal resistance profile compared to community-acquired strains and hospital-acquired strains circulating outside the ICU.
The high proportion of problematic fungi reduces the effectiveness of prevention and empirical treatment of candidemia with fluconazole in patients in the ICU, therefore, recently, clinicians are increasingly giving preference to alternative antifungal drugs - new azoles (voriconazole) and echinocandins.
In accordance with the latest clinical recommendations, azole drugs are used in stable patient conditions, in the absence of neutropenia, in the proven absence or low risk of resistant strains of Candida
(for example,
C. glabrata
,
C. krusei
) as an etiological factor. Otherwise, preference should be given to echinocandins [5].
Brief comparative characteristics of echinocandins
Echinocandins are semi-synthetic lipopeptides obtained by chemical modification of the fermentation products of molds: pneumocandin B 0
Glarea lozoyensis
(caspofungin), hexapeptide FR901370
Coleophoma empedra
(micafungin) and echinocandin B
0 Aspergillus nidulans
(anidulafungin).
Echinocandins are sometimes figuratively called antifungal penicillins because of their characteristic mechanism of action, which consists in inhibiting the synthesis of 1,3-β-D-glucan, which leads to osmotic lysis of the fungal cell as a result of damage to its membrane. Preparations of this group have high fungicidal activity against yeast fungi of the genus Candida
, including those resistant to other antimycotics, do not have a toxic effect on the macroorganism and are well tolerated. Unlike azoles, echinocandins have potential activity in biofilms [6].
All 3 echinocandins are characterized by higher minimum inhibitory concentrations (MICs) against C. parapsilosis
,
C. lusitaniae
and
C. guilliermondii
compared to other species of fungi of the genus
Candida
[7, 8].
In this case, MIC90 (concentrations that suppress the growth of 90% of cells) are in the range of <2 μg/ml. the greatest activity in vitro
, followed by micafungin and caspofungin [9]. It should be noted that at present, routine testing of the sensitivity of clinical fungal isolates to echinocandins is not recommended, since there is no direct correlation between MIC and clinical efficacy.
Echinocandins have low bioavailability when taken orally, so they are administered only parenterally. Compared to other echinocandins, anidulafungin has a larger volume of distribution (30–50 L) and a longer half-life (~26 h) [10]. The drugs do not create effective concentrations in the cerebrospinal fluid and urine, which should be taken into account for infections of the corresponding localizations.
Echinocandins do not have a significant effect on the pharmacokinetics of drugs metabolized via cytochrome P450 isoenzymes; they are not dialyzed; there is no need for dose adjustment in renal failure.
Unlike caspofungin and micafungin, which partially undergo biotransformation in the liver, the elimination of anidulafungin is due only to spontaneous chemical degradation to inactive peptide products excreted in bile. This determines its advantage in patients with liver failure [11].
Currently, caspofungin has the widest range of approved indications for use, as the drug that entered the market earlier than others and, as a result, has been the most well studied. However, the “younger” anidulafungin, due to its characteristics, has great clinical potential, which will undoubtedly be revealed over time.
Currently, the experience of clinical use of anidulafungin in our country is minimal. Below are 3 clinical examples illustrating the results of treating candidemia with this drug in cardiac surgery patients with a complicated course of the postoperative period.
Clinical example 1
Patient G., 53 years old, diagnosed with Epstein anomaly, concomitant pathology - subclinical hypothyroidism, arterial hypertension 2 degrees. high risk, NC 2A, FC 2, a defect correction operation was performed with tricuspid valve replacement with a biological prosthesis under artificial circulation.
In the early postoperative period, severe cardiac and respiratory failure was observed, which required the patient to stay in the intensive care unit for a long time. On the 14th day after surgery, ventilator-associated pneumonia developed ( Acinetobacter baumannii
), which was subsequently followed by acute renal failure, which required hemodiafiltration and liver failure with an increase in the level of bilirubin in the blood to 87.4 µmol/l.
Against the background of a complex of intensive therapy, including antibacterial therapy with cefoperazone/sulbactam and antifungal prophylaxis with fluconazole, positive dynamics of the patient’s condition and resolution of pneumonia were noted, which made it possible to wean the patient off mechanical ventilation and transfer her to the ward on the 25th day after surgery. On the 4th day after transfer, the condition is of moderate severity, hypothermia is noted at 35 ° C, a shift to the left in the leukocyte formula (up to 7% of band forms) with a leukocyte level of 13.3 × 109 / l, PCT - 0.73 ng / ml. Status localis
- diastasis and hyperemia of the edges of the sternotomy wound in the middle and lower third with scanty purulent discharge (superficial infection of the surgical site). Microbiological examination of blood cultures (taken by puncture and from the central venous catheter) revealed the growth of yeast fungi, identification and determination of sensitivity to antimycotics in the work. Also, the growth of yeast fungi was detected when inoculating wound discharge, urine discharged from the pharynx. The assessment of the severity of the condition according to the APACHE II scale is 5 points, according to SOFA - 6 points.
Considering the presence of a clinical picture of systemic inflammation in the patient against the background of a focus of infection, microbiological examination data and a low level of PCT, indicating against a bacterial etiology of the process, the central venous catheter was replaced with a new one, antifungal therapy with anidulafungin was started in the standard regimen (200 mg - loading dose, then - 100 mg IV drip once a day), against the background of which positive dynamics of the patient’s condition were noted. Already from the next day after the start of anidulafungin therapy, body temperature normalized; over the next week, regression of inflammatory changes was noted according to a clinical blood test. Candida albicans was detected in all examined materials
, sensitive to voriconazole, flucytosine and amphotericin B, moderately sensitive to fluconazole. The first negative blood culture was obtained on the 2nd day, sanitation of the urinary tract occurred on the 27th day of antifungal therapy. The course of treatment with anidulafungin was continued for 20 days, after which voriconazole was prescribed for another 1 week.
The patient was discharged in satisfactory condition, 2 months after the end of anidulafungin therapy, during a follow-up examination there were no clinical or laboratory signs of invasive candidiasis.
Clinical example 2
Patient K., 48 years old, underwent mitral valve replacement with a mechanical prosthesis and tricuspid valve repair due to rheumatic heart disease. Concomitant pathology - coronary artery disease, arterial hypertension 2 degrees. high risk. History: pulmonary embolism, post-infarction pneumonia. NK 2A, FC 3.
In the early postoperative period, the patient suffered an acute cerebrovascular accident of a mixed type in the left cerebral artery basin, against which asthenia, persistent respiratory failure, encephalopathy, and renal failure were noted; by the 15th postoperative day, ventilator-associated pneumonia ( Klebsiella pneumoniae)
, ESBL+), due to which the patient was on prolonged mechanical ventilation, complex treatment was carried out, including antibacterial therapy with meropenem, and hemodialysis procedures were performed repeatedly. Against this background, some positive dynamics were recorded, but severe respiratory failure persisted, and therefore the patient continued to be in the intensive care unit.
From the 30th day after the operation, the patient’s condition was serious, with negative dynamics associated with the appearance of signs of systemic inflammation (febrile fever up to 38.6 ° C, leukocytosis up to 18.4 × 109/l without a shift to the left in the leukocyte formula) in the absence of obvious source of infection. PCT test - 0.12 ng/ml. In the dynamics, renal failure persists - the level of serum creatinine reaches 183-204 µmol/l. The assessment of the severity of the patient’s condition on the APACHE II scale is 12 points, on the SOFA scale - 6 points.
Blood samples were taken (by puncture from a peripheral vein and from a vascular catheter), urine, separated from the pharynx and rectum for microbiological examination. The antibacterial therapy regimen was empirically adjusted (meropenem was discontinued, cefoperazone/sulbactam and linezolid were prescribed). The next day, the growth of yeast fungi was obtained in all studied samples.
Due to the development of invasive candidiasis in the patient against the background of an unstable condition and a clinical picture of systemic inflammation, the central venous catheter was replaced, and anidulafungin therapy was empirically started: 200 mg loading dose, 100 mg maintenance dose, once a day intravenously. The next day after the start of treatment with anidulafungin, the results of a microbiological examination were obtained; growth of Candida parapsilosis
(sensitive to amphotericin B, flucytosine and voriconazole, moderately sensitive to fluconazole), examination of throat discharge revealed the growth of
Candida krusei
(sensitive to amphotericin B and voriconazole, moderately sensitive to flucytosine, resistant to fluconazole). Taking these data into account, therapy with anidulafungin was continued. All subsequent blood cultures were sterile, but asymptomatic bacteriuria persisted for a long time, and therefore, after completing a 2-week course of anidulafungin, the patient was prescribed voriconazole orally for the next 14 days, after which negative urine culture results were obtained, the patient was discharged in satisfactory condition for further treatment in rehabilitation center. At a follow-up examination 3 months after the start of treatment with anidulafungin, the patient’s condition was satisfactory, he was feeling well, there were no clinical and laboratory data of a fungal infection, and renal failure had resolved. Residual neurological symptoms persist.
Clinical Case 3
Patient V., 74 years old, was admitted for surgical treatment for critical calcified aortic valve disease. Concomitant pathology - arterial hypertension 2 degrees, high risk, diabetes mellitus type 2, compensated by diet and oral administration of hypoglycemic drugs, duodenal ulcer (remission), chronic inactive viral hepatitis B. History of hysterectomy 10 years ago for malignant neoplasm.
The patient underwent aortic valve replacement with a biological prosthesis under conditions of hypothermic artificial circulation. The course of the early postoperative period was complicated by the development of acute cerebrovascular accident in the basin of the right middle cerebral artery, such as thromboembolism, with the development of left-sided hemiparesis and cerebral edema. Against the background of prolonged mechanical ventilation, ventilator-associated pneumonia developed ( Klebsiella pneumoniae
, ESBL+). Planned intensive therapy was carried out, including antibacterial therapy with meropenem, with positive dynamics of clinical and laboratory data on pneumonia. By the 14th day after the operation, a second wave of infection was noted: the appearance of persistent hyperthermia up to 38.9 °C was noted, inflammatory changes in the clinical blood test increased (leukocytosis 17.9 × 109/l, with a shift to the left up to 7% of immature forms) on background of low procalcitonin test values - 0.78 ng/ml. The assessment of the severity of the condition on the APACHE II scale is 22 points, on the SOFA scale - 9 points. Microscopy of urine sediment revealed yeast fungi. The development of systemic candidiasis is suspected. After taking blood cultures (puncture and from the central venous catheter), urine, and smears from the mucous membranes of the pharynx/rectum for fungi, the patient was empirically started on anidulafungin therapy (iv drip, once a day, loading dose - 200 mg, maintenance dose - 100 mg ). The next day, according to the results of a microbiological examination of the patient, the growth of yeast fungi was detected in all examined samples. The vascular catheter was replaced.
By the 3rd day of treatment, positive dynamics were noted - signs of systemic inflammation regressed, the PCT level decreased to 0.22 ng/ml. Microbiological examination data was obtained: growth of Candida parapsilosis
(sensitive to amphotericin B, flucytosine and voriconazole, moderately sensitive to fluconazole), culture of urine discharged from the throat and rectum revealed the growth of
Candida albicans
(sensitive to fluconazole, amphotericin B, flucytosine and voriconazole), taking this into account, therapy with anidulafungin was continued.
On the 11th day of treatment with anidulafungin, the patient again experienced a rise in body temperature against the background of abdominal pain with negative peritoneal symptoms and frequent loose, colitic stools. Colitis associated with Clostridium difficile
, for which vancomycin was prescribed orally; after 5 days the clinic was relieved.
The duration of therapy with anidulafungin was 14 days, after which, against the background of stabilization of the condition and positive dynamics of infection, de-escalation of therapy was performed with oral administration of fluconazole for another 7 days. After the start of antifungal therapy, when monitoring blood cultures, the latter remained sterile; fungi were no longer detected in urine cultures, starting from the 6th day of treatment with anidulafungin. The patient was discharged from the hospital in satisfactory condition; during a follow-up examination 3 months after discharge, there were no signs of recurrence of the fungal infection.
Conclusion
Initial clinical experience with anidulafungin indicates the effectiveness of this drug in patients with candidemia caused by strains with reduced sensitivity to fluconazole. The drug is well tolerated; no adverse drug reactions have been reported with anidulafungin treatment for up to 20 days. In our opinion, anidulafungin is a very promising treatment for invasive candidiasis, especially in patients with multiple organ failure or a high risk of developing it.
Information about authors
D. A. Popov
— Candidate of Medical Sciences, Head of the Laboratory of Clinical Microbiology and Antimicrobial Therapy
Place of work: Federal State Budgetary Institution Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev", Moscow
T. Yu. Vostrikova
Place of work: Federal State Budgetary Institution Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev", Moscow
How is the procedure performed?
The procedure rarely takes more than thirty minutes in the case of X-ray densitometry and fifteen in the case of ultrasound. All the patient needs to do is take a certain position on a special diagnostic table. A detector will be located above the area under study. If you don't know how bone densitometry is performed, it's worth knowing that the sensor can be moved over different areas of the patient's body. The level of transmission of rays through the body is measured and recorded by a special program, after which the data is subject to processing. Sometimes parts of the patient's body are fixed with special devices to reduce their mobility to zero, and the person is also asked to hold his breath to get the clearest possible image.
Inpatient study
It is important to learn what densitometry is, what the procedure is and what to expect from it before undergoing such an examination. You can undergo diagnostics in a doctor's office using a stationary device. It is a special table with sensors on which the patient needs to lie down.
Monoblock equipment
People often ask the question: “Densitometry: what is it, how is it done?” when they are prescribed such a study. Diagnostics can also be performed using portable equipment. However, this does not mean that the procedure can be performed outside a diagnostic center, since it involves x-rays. Using monoblock equipment, it is convenient to examine the bones of the phalanges of the fingers and heel.