Previous Next Magnetic resonance imaging of the knee joint is one of the preferred methods for diagnosing most articular pathologies of the knee area. During MR scanning, it is possible to successfully identify various types of degenerative changes and inflammatory processes at an early stage, including bone fractures, damage to cartilage tissue and soft structures of the muscular and ligamentous apparatus. A tomograph scan of the knee is non-invasive. The patient does not experience any discomfort, the examination is not dangerous to his health and can be carried out repeatedly if necessary. An MRI of the knee joint can be done either upon the doctor’s direction or on the patient’s personal initiative.
- MRI
- Ultrasound
MRI tomograph:
Siemens Magnetom C
Type:
Open (expert class)
What's included in the price:
Diagnostics, interpretation of images, written report from a radiologist, recording of tomograms on CD + free consultation with a neurologist or orthopedist after an MRI of the spine or joint
Ultrasound machine
HITACHI HI VISION Avius
Class:
Expert (installation year 2019)
What's included in the price:
Diagnostics, interpretation of images, written diagnostic report
What is magnetic resonance imaging of the knee joint
Magnetic resonance imaging of the knee is a scanning technique in which images are obtained using the physics of the phenomenon of nuclear magnetic resonance. During the examination, the patient's knee is placed inside a tomograph, where a strong magnetic field is created and radio frequency pulse sensors work. Under this influence, hydrogen atoms in tissue cells begin to perform oscillatory movements. This resonance is recorded by the installation computer, digitizes the data and converts it into three-dimensional images of a black and white spectrum. The more water is contained in the tissues of the examined area, the more contrast and clarity the scans will be. Muscles, tendons, and cartilage contain enough water, so these tissues are very well visualized on tomograms. Bones have little water in their structure, so they are poorly detailed in photographs. A more effective method for diagnosing bone pathologies of the tibia and femur will be computed tomography.
MRI for arthrosis in Moscow
Of course, it is impossible to give an exact answer to the question which method of diagnosing arthrosis is better: it all depends on the patient’s condition, his medical history and financial capabilities. However, many doctors agree: MRI of joints for arthrosis is the most advantageous option due to its safety and high image quality.
Do you want to undergo an MRI of joints in Moscow? Sign up for our Elena Malysheva Diagnostic Center! At your service is a modern expert-class tomograph, experienced specialists with many years of experience and affordable prices!
Sign up for diagnostics at the Elena Malysheva Diagnostic Center near the Baumanskaya metro station (see map) by phone or leave a request on the website.
Baumanskaya metro station (see map) 8
leave a request on the website
Indications
The following symptoms may make you think about the need to do a magnetic resonance imaging scan of the knee joint:
- persistent pain in the knee;
- swelling of the skin and swelling;
- accumulation of blood and suppuration in the joint capsule;
- change in the shape of the knee;
- problems bending or straightening your leg;
Patients who are planning knee surgery are often asked to do an MRI. Tomography data allows us to evaluate the anatomical features of the patient’s knee joint and build the correct surgical plan.
Initial appointment with an ORTHOPEDIST
ONLY 1800 rubles!
(more about prices below)
Expert equipment
The Clinical Hospital on Yauza uses the latest generation 1.5 T Philips Ingenia fully digital magnetic resonance imaging scanner, which provides:
- Reduced scanning time (less time to lie in the magnet)
- Maximum possible tunnel diameter (73 cm)
- Highest quality images
- Full range of studies due to maximum equipment
- Additional information through advanced software
- Environmental control system (music from the patient’s playlist, choice of lighting, personal climate control)
- Automated quality control system for research and descriptions
- IT platform with triple control of research results - with the support of professors, leading specialists from Russia, Europe and Israel (“second opinion”)
Deciphering and preparing a medical report usually takes about 20 minutes after the diagnostic procedure. In complex cases, to increase the reliability of the research results, the description time can be increased. Images are written to disk or flash card. At the patient's request, it is possible to print images on film (additional charge)
What will an MRI of the knee show?
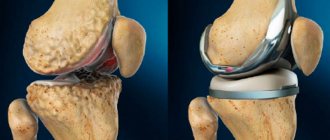
The structure of the knee joint includes very diverse tissues: ligaments, tendons, bones, fatty tissues, cartilage. All of them are subject to inflammatory or degenerative changes. MRI of the knee joint allows for a comprehensive assessment of changes in the ligamentous apparatus, menisci, and bone structures that form the joint. Most often the knee suffers from:
- bone-traumatic injuries;
- degenerative changes in cartilage tissue (menisci, articular cartilage);
- ligamentous injuries;
- osteochondropathy;
- necrosis, arthrosis and arthritis;
- tendinitis.
Tomogram data will help to make a differential diagnosis of these diseases, assess the degree of damage to the articular apparatus and build a prognosis for possible treatment and recovery of the patient. If the patient has undergone active therapy, using a series of MRI images, the doctor can conduct a comparative analysis and assess the degree of progress or regression.
MRI after knee injury
MRI of the knee is one of the most effective ways to diagnose knee injuries. According to the World Health Organization, 80% of people in the world suffer from this or other diseases of the musculoskeletal system. Some scientists believe that diseases of the joints and spine are humanity’s retribution for upright walking. Whether this is true or not is difficult to say. But the fact remains that half of the people on the planet will sooner or later encounter pathologies of the knee joint, especially if you are a fan of active sports. Up to 50% of all sports injuries are related to knee damage.
If a knee injury has occurred in your life, an orthopedist will most likely give you a referral for magnetic resonance imaging, since it shows much better the soft tissues, ligaments and tendons, which are much more often and more easily injured than the bone component of the joint. An MRI scan is a safe test due to the absence of x-rays, unlike computed tomography (CT) and radiography. MRI is the only method that provides comprehensive information about a knee injury such as a subchondral (hidden) fracture. This type of fracture is called occult because its signs remain invisible on x-rays and arthroscopy. On an x-ray, this joint will appear undamaged. Meanwhile, this knee injury requires prompt treatment to avoid secondary degenerative changes in the cartilage.
Previous Next
MRI for meniscal damage
Damage to the meniscus (meniscopathy) is one of the most common knee injuries. Most meniscus damage happens, as they say, out of the blue. For example, an unsuccessful leg movement or squatting can be associated with this grass. When the meniscus is pinched or torn, the patient experiences sharp, stabbing pain in the knee. After such an injury, the leg usually swells. With such symptoms, the patient should come to see an orthopedist and have an MRI of the knee joint. Based on its results, the doctor will be able to assess the extent of the damage and answer the question of whether the damaged meniscus requires surgical intervention.
MRI for Baker's cyst
In addition to damage to the meniscus, a person may suffer from a phenomenon called Baker's cyst. It forms when the stretched capsule of cartilage in the knee bulges back and fills with synovial fluid. This cyst does not necessarily cause pain, but always limits movement. The patient feels that the knee cannot be fully bent.
The Baker's cyst can be independently felt by the patient under the knee in a bent position. Usually this tumor does not cause severe pain and is benign. But at some point, the popliteal cyst can fester and lead to purulent arthritis. This protrusion can also cause venous thrombosis. Therefore, it is important that a Baker's cyst is diagnosed and removed. Magnetic resonance imaging will again help in diagnosing the exact location of the popliteal wrist.
Alternative research methods
- CT of the knee joint is a method with high resolution in assessing bone structures, but has its limitations in assessing soft tissues and ligaments.
- X-ray is a method that also evaluates bone structures, but has a lower radiation dose and resolution than CT.
Contraindications Preparation
How often should you have an MRI of your knee?
Typically, magnetic resonance imaging of the knee joint is prescribed only if the patient has suffered an injury or has pain. However, there is a group of people for whom knee imaging is recommended on a regular basis. Sport is not only about medals and victories, but also about grueling hours of training and daily testing of the body’s strength. With increased stress on the body and sports-related injuries, it becomes extremely important to monitor any changes in the condition of the athlete’s musculoskeletal system. This is where MRI comes to the rescue. The general recommendation of doctors for people leading an active sports lifestyle is to conduct an MRI of the entire spine and an MRI of joints that are subject to heavy load due to sports at least once a year.
Tumor diseases of the knee
Benign neoplasms or cancer can occur in the area of the knee joint, including the development of metastases of tumors located in other parts of the body (lungs, breast, prostate gland).
The most common tumor, osteosarcoma, affects the tibia or femur. Chondrosarcoma is a little less common; it affects the cartilaginous surfaces of the joint and the menisci. Benign tumors of the knee joint - chondroma, osteoclastoma, cyst.
Tumors develop unnoticed, often without any symptoms in the initial stages. The only sign of the development of the disease may be the appearance of a tumor-like growth, but not in all cases. Later, pain, swelling of the knee, and signs of intoxication of the whole body occur. The rate of tumor growth, as well as the manifestation of symptoms, vary from person to person.
In the later stages, a successful outcome is unlikely, so it is necessary to detect the tumor and begin treatment as early as possible.
MRI for tumor tumors is a method of early diagnosis, allowing timely treatment to be prescribed and a stable positive result to be obtained.
In the photographs you can see swelling, areas of bone deformation with a heterogeneous structure—foci of decay in osteosarcoma. Chondrosarcoma will be characterized by a lobular structure with septations and dense inclusions. Benign tumors and cysts have a more uniform structure.
How to do a tomography of the knee
The magnetic resonance imaging procedure takes place in a comfortable environment for the patient. In most diagnostic centers in St. Petersburg, it is carried out by appointment. Before entering the MRI room, the subject will be asked to remove all metal objects from the body and remove all electronic devices from their pockets. A tomograph is a big magnet. Having metal objects near him may cause him to attract them towards him. In addition, the presence of metal in the scanning area reduces the quality of the images.
The second factor that affects the quality of magnetic resonance imaging is the immobility of the patient. In the diagnostic room, he will be asked to lie down on a mobile table, a special intensifying coil will be put on his knee and brought inside the scanning part of the tomograph. The patient will be asked to remain still throughout the examination. The average screening duration is 30 minutes. Usually the patient does not feel anything other than slight heating in the examination area. The only thing that can be annoying is the noise of a working tomograph. If it is too strong, a person can always ask to be given noise-canceling headphones.
Questions about diagnostics
Dress code
You can enter the MRI room in any clothing that does not contain metal. When going to the clinic, it is best to wear loose, non-restrictive clothing without metal elements (zippers, rivets, hooks), in which you can lie comfortably. For women, we recommend bringing a T-shirt or not wearing a bra with metal wires or hooks.
Preparation
This tomography does not require any preparatory steps from the patient.
Is MRI harmful to health?
MRI is a completely harmless diagnostic method for the human body. This method of examination can be carried out at any age and for any disease an unlimited number of times, unless you have contraindications.
Contraindications
Some pacemakers and foreign objects in the body may pose serious limitations to tomography. In particular, cochlear implants, vascular clips, stents, heart valves and insulin pumps, pacemakers, neurostimulators, steel screws, staples, pins, plates, joint endoprostheses may be a contraindication to diagnosis. The patient must notify the radiologist about all implanted objects in the body. The diagnostician will be able, based on information about the composition and model of the implant, to assess the possibility of conducting diagnostics.
If you are having an MRI with contrast, be sure to report any allergies to medications or kidney problems. It is also necessary to inform the radiologist about a possible pregnancy.
Is it possible to do an MRI with braces and dental implants?
Dental implants and crowns are not a contraindication to magnetic resonance imaging. The magnetic field does not have any negative effect on them. Fixed brace systems can produce artifacts on tomograms during MRI of the head. If the light effect is too strong, the doctor will stop the study and offer the patient alternative diagnostic methods.
Is the device noisy?
Any MRI machine in working condition makes noises reminiscent of tapping. The open tomograph is one of the quietest installations. The noise from its operation is significantly lower compared to closed tomographs. If the sounds of the operating unit cause you anxiety, you will definitely be offered special noise-canceling headphones.
What should I do if I have claustrophobia?
An open tomograph is the optimal solution for patients suffering from panic attacks in a closed space. It is open on the sides on three sides and does not create a claustrophobic feeling.
Can I take sedatives before an MRI?
If you are a little nervous, before the tomography you can take mild sedatives, for example, valerian, motherwort infusion or afobazole. Taking sedatives does not have a negative impact on the quality of MRI.
Why is it important not to move during the test?
Any movement during the examination reduces the quality of the resulting images. Multiple motion artifacts may appear on the images, and the MRI results will be uninformative.
Can I do the research with an accompanying person?
Absolutely yes. You can invite any accompanying person from among your family and friends to the MRI room. It is important that your companion does not have metal implants or artificial pacemakers in his body.
What is MRI with contrast?
To get clearer images, the patient is sometimes prescribed a special substance before the procedure. It does not pose a danger to the body and performs one single function - to illuminate and better visualize the organ being examined. The dye has no contraindications for use, is quickly eliminated from the body and does not cause allergic reactions. In isolated episodic cases, there is a slight rash and slight dizziness (up to 0.1%) caused by individual intolerance to the drug.
Most often, contrast is administered intravenously. The substance includes iron oxide, which most effectively visualizes blood vessels. However, this method is in demand not for diagnosing joints, but, for example, for multiple sclerosis.
If the gastrointestinal tract is to be examined, oral contrast based on manganese compounds and gadolinium soda is used. Sometimes green or blueberry tea, which contains a high concentration of manganese, is used as a contrast agent. For joint diseases, MRI with contrast is most often not prescribed.
MRI with contrast is performed in 20% of cases – for gastrointestinal pathologies, suspected oncology and diseases of the spine
Decoding
The results of the tomography will be black and white images in three-dimensional format. They are deciphered by a radiologist. He carefully evaluates the anatomical features of the patient’s knee structure and notes all the anomalies found in his conclusion. The conclusion, together with MRI images printed on film or recorded on electronic media, is handed over to the person being examined. The decryption procedure takes on average 40-60 minutes. In complex and controversial cases, doctors are sometimes forced to resort to a second independent opinion. This is a situation where the patient’s images are additionally assessed by a radiologist of the highest category and expresses his independent opinion on the accuracy of the diagnosis. With the tomography data, the subject must make an appointment with his or her attending physician. It is he who, summing up all the data on the medical history, the results of analyzes and tests, makes the final diagnosis and proposes a treatment strategy.
An example of MRI decoding of the knee joint
On a series of MRIs of the right knee joint, the relationships in the joint are not disturbed.
In the area of the upper inversion and lateral pockets, an accumulation of effusion is determined in the joint cavity. The synovial membrane is hypertrophied. In the anterolateral sections, at the pre- and infrapatellar level, areas of edema of the subcutaneous fatty tissue are determined.
The patella is in the middle position. MR signal from the subchondral parts of the patella without pathological changes. The ligaments holding the patella are not changed. Hoff's fat body has a homogeneous structure. The patellar ligament has a homogeneous structure, the area of the tibial tuberosity is not changed.
The cartilaginous covering of the condyles of the femur and tibia is unevenly thinned, the articular cavity is moderately narrowed, and is more pronounced in the medial part of the joint. The bone contour of the condyles of the femur and tibia is not deformed. In the postero-central internal sections of the medial condyle of the tibia, a local area of cyst-like restructuring is identified subcortically, without pathological changes from adjacent trabecular sections. Small antero- and posterolateral marginal bone growths of the condyles of the femur and tibia are identified.
The anterior cruciate ligament is defined throughout its entire length, its structure is heterogeneous, the contour of the ligament is clear, and its overall integrity is preserved. Extrusion of the medial meniscus and an increase in the intensity of the MR signal from the posterior horn of the meniscus, with signs of damage, are determined. The intensity of the MR signal from the lateral meniscus, posterior cruciate and collateral ligaments is not changed, their integrity is not compromised.
In the posteromedial thigh, in the area of the intermuscular space of the medial head of the gastrocnemius and semimembranosus muscles, a cystic expansion of the mucous bursa is noted.
Conclusion:
MRI signs of grade 2 deforming arthrosis of the right knee joint; damage to the posterior horn of the medial meniscus; degenerative changes of the anterior cruciate ligament. Synovitis. Baker's cyst.
How is the examination carried out?
The duration of the MRI procedure ranges from 20 to 60 minutes, depending on the area being examined, the extent of the pathology and the need to use a contrast agent. Before the examination, you must inform your doctor about your suspicions about the presence of contraindications, if any. For example, if a woman suspects early pregnancy, it is better to postpone an MRI.
During the examination, the patient will have to lie still, since only if this condition is met is it possible to obtain a high-quality image. If the pain, for example due to arthrosis of the hip joint, is too strong or aching, special painkillers or sedatives may be administered before the session.
The patient is placed on a special couch, his legs, arms and head are fixed to prevent involuntary movements during the scan. The table slowly moves into the tomograph - a device in the form of a large hollow cylinder. Since the tomograph produces sharp loud sounds, during the examination the person is asked to wear earplugs or headphones with calm music.
MRI results will be ready in a few hours
Contraindications
Since MRI examinations are performed using a magnetic field, you need to remember that metal objects in a magnetic field can move and heat up. Therefore, the presence of metal in the body is a limitation to MRI scanning.
A pacemaker will also be a contraindication for diagnosis. In a strong magnetic field, any electronic devices may fail or their operation may be impaired. If there is an electronic device in the body, you need to consult a doctor about the possibility of performing a tomography.
When patients come for an MRI, the question is often asked: are crowns and dental implants a contraindication? And the answer in most cases will be no. Modern dentures are mostly made of non-magnetizable material and will not be a limitation in tomography.
Author: Belik Ekaterina Mikhailovna
Radiologist with 19 years of experience
What does the price of magnetic resonance imaging of the knee depend on?
The cost of an MRI of the knee joint is determined by several basic factors:
the power of the tomograph, which is measured in Tesla;
- the need to use contrast enhancement;
- personnel qualifications;
- availability of discount promotions.
The most inexpensive way to do a tomography of the knee is to use open machines. The most accurate and most expensive scanning will be an examination using an ultra-high-field tomograph with an induction power of 3 Tesla.
| Service | Price according to Price | Discount Price at Night | Discount Price During the Day |
| from 23.00 to 8.00 | from 8.00 to 23.00 | ||
| MRI of the knee joint | 4000 rub. | 3190 rub. | 3690 rub. |
| Appointment with an orthopedist | 1800 rub. | free after MRI | free after MRI |
| First aid program for joints (8 studies + appointment with an orthopedist + MRI of the joint) | 13000 rub. | 7500 rub. | 7500 rub. |
What determines the cost of tomography?
Tomograph power
Applying Contrast
Personnel qualifications
Promotions and discounts
What are the contraindications for MRI?
For some diseases and special conditions, the joint cannot be examined using MRI. Among them:
- severe claustrophobia (if the patient is afraid of tight spaces, he will not be able to spend a long time under the influence of the device);
- first trimester of pregnancy (risks outweigh expected benefits);
- epilepsy;
- the presence of metal structures in the body - implants with metal components or prostheses on metal pins (metal can distort the readings generated by magnetic waves);
- presence of a pacemaker, inner or middle ear implant, insulin pump.
MRI is absolutely safe - there is no ionizing radiation
Interpretation of results when diagnosing the knee on MRI
It is handled by an experienced diagnostician. Examining the obtained images, he carefully determines the nature and extent of the spread of the pathology and describes the structural features of the joint structures. For this purpose, special schemes and protocols are used. Sometimes it takes several hours to draw up a conclusion. The doctor states:
- what is the condition of the cartilage tissue, ligaments, cords connecting the bones and the meniscus;
- description of blood vessels and abnormalities present in them;
- the presence of degenerative and dystrophic changes resulting from metabolic disorders;
- presence and amount of liquid;
- tumors of a benign or malignant nature.
The patient receives serial images and a final diagnosis based on them. The specialist involved in your treatment can tell you in detail about your health condition. He will study the images and determine how to proceed in a specific clinical case: prescribe therapy, after which he will repeat the MRI or refer you for further examination or to another competent doctor. You can't self-diagnose. Contact a qualified specialist and medical assistance will be timely and correct. Do not delay your visit to the clinic. Patients who neglect their health subsequently suffer from complications of an untreated disease.
Decoding the results
The images are interpreted by a highly qualified doctor of rheumatology, traumatology or orthopedic specialization. For description, three-dimensional images are provided, where the structure of the joint and nearby tissues is visible layer by layer. Only a competent specialist can decipher the result; do not try to interpret the result yourself. If no deviations are observed, the doctor will indicate in conclusion that the joint is located anatomically correctly, has no ruptures or damage, the volume of synovial fluid is normal, there are no neoplasms, and no pathological changes have been identified.
If the test reveals abnormalities, your doctor will discuss possible treatment options with you.
Advantages of diagnostics using MRI
If you carry out the procedure after consultation with a doctor (i.e., exclude the presence of contraindications), you can confidently say that MRI does not harm the body and is the most informative diagnostic procedure. Magnetic fields do not have a negative effect on the human body, for this reason MRI of the knee joint can be performed repeatedly with minimal intervals. Another significant advantage is its non-invasiveness (unlike, for example, arthroscopy).
Other advantages are:
- Lack of complex preparation;
- Minimum list of contraindications;
- Quick receipt of research results;
- Relatively fast diagnostic process;
- No pain or discomfort.
MRI can act as an independent study or as an additional one, for example, to confirm a presumptive diagnosis after ultrasound or CT.