Damage to the lateral ligaments of the knee joint
The lateral or collateral ligaments of the knee joint are located, according to their name, along its lateral surfaces.
The external lateral or collateral fibular ligament begins from the external epicondyle (bone protrusion) of the thigh. It covers and strengthens the knee joint from the side. Below this ligament is attached to the head of the fibula. A layer of fatty tissue separates the lateral ligament from the joint.
The external collateral ligament of the knee joint is damaged less frequently than the internal one, but more often the entire ligament is torn completely or the ligament is completely torn from its attachment.
The internal lateral or collateral tibial ligament is subject to traumatic injuries more often.
However, it usually ruptures partially. This ligament starts from the inner femoral condyle. It looks like a wide band, covers and strengthens the inner surface of the knee joint, and below is attached to the tibia. In addition, some of the fibers of the internal collateral ligament are woven into the joint capsule and into the tissue of the internal meniscus of the knee joint. This attachment of the ligament leads to possible damage to the inner meniscus of the knee joint when the ligament is injured.
Damage to the collateral ligaments occurs as a result of tension when the tibia deviates. If the shin deviates outward (when walking on an uneven surface, tucking the foot in a heel, etc.), the ligaments are subject to strong tension and are torn or torn. If the tibia deviates outward, the internal ligament ruptures, and if the tibia deviates inward, the lateral collateral ligament of the knee joint is damaged.
When the lateral collateral ligament is torn, an avulsion fracture of the portion of the head of the fibula to which the ligament attaches may occur. Patients complain of pain in the area of the rupture, which intensifies when trying to deviate the leg outward when the internal ligament is torn, or inward when the external ligament is torn. Partial ligament ruptures result in limited flexion in the knee joint, while complete ligament ruptures lead to excessive mobility (looseness) in the joint. The diagnosis is clarified using x-rays taken with special placement of the legs.
Content
- 1 Main signs of tibial collateral ligament rupture
- 2 Prevention
- 3 Clinical picture 3.1 History and complaints
- 3.2 Physical examination
- 3.3 Radiation diagnostics
- 3.4 Special methods
- 9.1 History and complaints
- 10.1 Conservative treatment
Clinical picture[edit | edit code]
A rupture of the tibial collateral ligament is characterized by pain in the medial part of the knee joint. The typical mechanism of injury is either a rotational non-contact or a direct blow directed from the outside to the inside. Joint instability is a variable symptom and depends on the severity of the injury.
History and complaints[edit | edit code]
It is very important to find out when and where the injury occurred. Incomplete ruptures (I or II degree) usually occur as a result of non-contact rotational trauma, complete (III degree) - due to an external blow to the thigh or upper leg. The presence and localization of pain and instability, the timing and rate of increase in swelling, the sensation of a click or crack are clarified. Paradoxically, I and II degree tears are often more painful than complete tears. Rapidly increasing swelling indicates concomitant cruciate ligament injury, patellar dislocation, or fracture.
When evaluating patients with knee injuries, look for previous injuries or a history of joint instability.
Physical examination[edit | edit code]
If a tibial collateral ligament injury is suspected, the knee joint is examined completely to ensure that no associated injuries are missed. This is especially important with regard to the cruciate ligaments, since an injury to any of them significantly alters the course of treatment. A combination with a dislocation of the patella is very common, therefore, in addition to standard tests to assess its condition, the patella itself and the ligaments that support it on the medial side must be palpated.
At the site of the rupture, along the medial surface of the joint, there is usually pain on palpation. Joint instability during the abduction test is assessed by the expansion of the joint space in the medial part with the knee bent at an angle of 30°. The latter condition is especially important, since in a fully extended joint the posterior part of the joint capsule and the posterior cruciate ligament resist the valgus load and do not allow the detection of damage to the tibial collateral ligament. Normally, the articular surfaces fit tightly to each other, their discrepancy by 1–4 mm corresponds to grade I tears, by 5–9 mm to grade II tears, and by 10–15 mm to a complete tear. In addition, with ruptures of the I-II degree, an obstacle to further separation of the articular surfaces is clearly felt, while with a complete rupture, the obstacle is almost not felt.
Radiation diagnostics[edit | edit code]
If a serious injury to the knee joint is suspected, a complete x-ray examination is required. Radiographs look for fractures (including Segon's fracture; see Radiology for Anterior Cruciate Ligament Injuries), as well as articular mouse, Pellegrini-Stida syndrome (calcification of the tibial collateral ligament), and patellar luxation. In children and adolescents, functional radiography is performed to exclude Salter-Harris fractures.
MRI is better suited to clarify the location of the tibial collateral ligament tear and identify concomitant meniscal tears and damage to other articular structures. Relative indications for MRI include suspicion of anterior cruciate ligament injury if it cannot be excluded by other methods, suspicion of a meniscus tear, and preparation for surgical repair of the tibial collateral ligament.
Special methods[edit | edit code]
If the patient is afraid of pain and intuitively tenses his muscles during examination, he can be examined under anesthesia. Arthroscopy is also used to identify associated injuries. However, almost always these diagnostic methods are replaced by MRI, which is primarily used in this clinical situation.
Basic principles for diagnosing knee ligament ruptures:
Modern diagnostic equipment and the clinical experience of traumatologists at the Sourasky Medical Center make it possible to make the correct diagnosis and identify the exact location of the rupture without much difficulty.
- Inspection and palpation of the knee joints.
- X-rays of the knee joint (to exclude fractures of the tibia or femur).
- Ultrasound scan of the joint (to confirm hemarthrosis).
- Magnetic resonance imaging (to exclude meniscal tears).
- Diagnostic arthroscopy (to identify ruptures of intra-articular cruciate ligaments, with the possibility of surgical suturing).
Treatment[edit | edit code]
Treatment of isolated damage to the tibial collateral ligament is usually conservative and consists of eliminating the valgus load and early mobilization of the joint. Classic surgical techniques, previously widely used, are in no way superior to this method.
I-II degree tears are treated with a plaster cast or splint; the use of crutches is not necessary if the patient can lean on his leg. It is allowed to bend the leg at the knee joint after 1-2 weeks; The sooner the range of motion is restored, the faster the rehabilitation proceeds.
Treatment tactics for third-degree ruptures are not so clear. Studies have shown that joint instability often persists after conservative treatment, although in most of these cases injury to multiple ligaments could not be ruled out. If we compare the results of conservative and surgical treatment for isolated complete ruptures of the tibial ligament, then here too the conservative approach has advantages both in terms of the subjective sensations of patients and in terms of rehabilitation time.
When third degree ruptures are combined with ruptures of other ligaments, it is impossible to do without surgery. In such cases, especially when the distal end of the tibial collateral ligament is torn from the bone, the results of conservative treatment are not nearly as good as for isolated injuries of this ligament. Immediately after the injury, the ligament is sutured and, if necessary, shortened, the torn sections of bone are put back in place and fixed. If the remaining parts of the ligament are not enough for a complete restoration, additional plastic surgery is performed with an auto- or allograft. This need arises especially often with delayed intervention.
As a rule, the application of a plaster cast or surgical treatment significantly delays the start of exercise therapy to restore range of motion. With conservative treatment using a functional splint and early mobilization, strengthening of the ligaments and restoration of joint mobility occur much faster (of course, in the absence of valgus load). After improving joint mobility, static exercises begin. Their intensity increases as the limb strengthens.
TREATMENT
An isolated tear of the lateral or medial collateral ligament rarely requires reconstructive surgery. In these cases, conservative therapy is carried out, which consists of fixing the lower limb extended at the knee joint using a brace or plaster cast. However, many traumatologists prefer not to use external immobilization of the knee joint for an isolated rupture of the medial collateral ligament. Although there is an opposite point of view: external immobilization means should be used for any injury to the knee joint, accompanied by pain and symptoms of instability. Initial treatment for a collateral ligament tear is aimed at reducing pain and traumatic swelling. To do this, it is necessary to rest the injured limb and apply ice packs to the knee joint area. In case of significant injury, it is recommended to take anti-inflammatory drugs (diclofenac, aspirin, ketonal, etc.). When walking, you must use crutches until the lameness disappears.
To reduce pain in the acute period, the use of transcutaneous electrical nerve stimulation (TENS) may be indicated. After severe pain subsides and swelling decreases, physical therapy is added to the complex of conservative therapy. The purpose of physical therapy is to restore the normal range of motion in the damaged joint and restore the strength of the muscles of the limb (especially the quadriceps muscle located in the anterior region of the thigh). It has now been shown that early administration of physical therapy leads to a more rapid and complete restoration of knee joint function and a reduction in the overall duration of the rehabilitation period. If, after restoring muscle strength and joint function, the patient still has symptoms of instability, the patient must use external immobilization devices (braces) during physical activity. In some cases, the surgeon may offer you surgical treatment.
Surgical treatment is usually indicated for combined damage to the collateral ligament and other structures of the knee joint. Some surgeons believe that with a combined rupture of the medial collateral and anterior cruciate ligaments, surgery is necessary to restore the function of both ligaments. Other experts disagree with this opinion. They propose to perform anterior cruciate ligament replacement after a course of conservative treatment aimed at restoring the integrity of the collateral ligament. Time will tell which approach is optimal. During reconstructive surgery, a skin incision is made in the area of projection of the torn collateral ligament. If the ligament is torn off in the area of its attachment to the bone, then the ligament is fixed using metal fixators or strong synthetic threads. In case of a median rupture of the collateral ligament, the ends of the ligament are sutured to each other. With “old” ruptures, suturing of the collateral ligament is in many cases not possible due to the appearance of scar changes in the torn ligament. To eliminate instability of the knee joint in these cases, the torn collateral ligament is replaced with an autograft. What it is? An autograft is a piece of ligament or tendon that is taken from another location from a patient during surgery. In most cases, the tendon of the semitendinosus muscle, one of the muscles of the posterior thigh, is used as a graft. Recent studies have shown that harvesting of the semitendinosus tendon does not result in decreased lower extremity strength due to compensatory hypertrophy of other thigh muscles. The ends of the autograft are attached to the bone using metal screws or strong synthetic threads.
Complications[edit | edit code]
The transition to predominantly conservative treatment significantly reduced the number of complications associated with injuries of the tibial collateral ligament. The main complication of conservative treatment is weakness of the ligamentous apparatus during valgus loading and pain in the medial part of the joint. Radiographs may reveal residual calcification of the ligament (Pellegrini-Stida syndrome). After surgical treatment, cicatricial deformation of the joint, inflammation, damage to the saphenous nerve and vein, and weakness of the ligamentous apparatus are possible.
Treatment of medial collateral ligament rupture
To confirm a rupture of the medial collateral ligament and diagnose damage to other structures of the knee joint, a competent orthopedic traumatologist will definitely prescribe radiography in two standard projections and recommend MRI (magnetic resonance imaging) of the knee joint.
If only the medial collateral ligament of the knee joint is damaged, the traumatologist will recommend conservative treatment. It consists of immobilizing the knee joint in a comfortable straight orthosis, which makes flexion and extension of the knee joint impossible. In addition, the doctor will recommend elastic bandaging or wearing compression stockings, as well as special medications that prevent the formation of blood clots in the veins. This is critically important, since any injury to the lower limb can provoke deep vein thrombosis, so it is necessary to regularly visit the doctor for follow-up examinations and strictly follow the recommendations. If you follow the recommendations of a competent and experienced orthopedic traumatologist, the medial collateral ligament heals in 3-4 weeks, depending on the degree of initial damage. Further, after the cessation of immobilization and the beginning of active movements, for the first time, patients are recommended to use a special stabilizing knee brace to prevent re-injury of the internal collateral ligament.
Conservative treatment
In rare cases, the medial collateral ligament is damaged at its attachment site (usually the attachment to the femur) and a bone fragment is torn from the femur. Depending on the degree of initial displacement, conservative treatment is acceptable, but refixation of this bone fragment to the femur with screws is recommended.
In cases of incomplete healing of the medial collateral ligament of the knee, with continued uncertainty when walking and playing sports, if the initial recommendations were not followed or the wrong treatment tactics were chosen, an experienced traumatologist will recommend surgical treatment. Some surgeons recommend initial surgical restoration of the medial collateral ligament using an autograft (the patient's own tissue), but only in cases of the most massive damage (this is grade III according to the MRI classification). Surgical intervention consists of repeating the anatomy of the internal collateral ligament with a tendon autograft, which is simultaneously fixed in the femur and tibia. This ensures proper stability of the knee joint, and the patient again has the opportunity to quickly return to an active lifestyle and usual physical activity, which is extremely necessary in the modern and dynamic world.
If damage to the internal collateral ligament is accompanied by other injuries to the knee joint, then the decision is made by both the patient and the traumatologist, based on the patient’s preferences, his age and the desired level of physical activity. It is very important to contact a competent orthopedic traumatologist, because this is the only way to formulate the right treatment tactics for a speedy return to an active lifestyle. As a rule, when the medial collateral ligament of the knee and the anterior cruciate ligament are simultaneously damaged, it is first recommended to heal the medial collateral ligament of the knee joint, then develop movements in the knee joint, and only then arthroscopic plastic surgery of the anterior cruciate ligament. This required waiting time is important to prevent postoperative complications such as stiffness (significant limitation in the range of motion of the knee joint).
Surgery for medial knee ligament rupture
If the medial collateral ligament and medial meniscus are simultaneously damaged, it is permissible to perform arthroscopic resection (removal) or suturing of the damaged part of the meniscus, followed by immobilization of the knee joint for the same period (3-4 weeks), which is due to the less traumatic nature of the operation associated with the meniscus.
With timely and correct diagnosis and correctly chosen treatment tactics, both isolated and combined damage to the medial (internal) collateral (lateral) ligament of the knee joint cannot be a limitation to an active lifestyle and favorite sports activities.
Prognosis and return to sports[edit | edit code]
For isolated injuries of the tibial collateral ligament, conservative treatment usually gives good results. Thus, 98% of football players with an isolated injury to the tibial collateral ligament who underwent conservative treatment returned to professional sports.
Literary sources:
- Gardiner JC et al: Strain in the human medial collateral ligament during valgus loading of the knee. Clin Orthop Related Res 2001;391:266.
- Mazzocca AD et al: Valgus medial collateral ligament rupture causes concomitant loading and damage of the anterior cruciate ligament. J Knee Surg 2003; 16(3): 148.
- Nakamura N et al: Acute grade 111 medial collateral ligament injury of the knee associated with anterior cruciate ligament tear. The usefulness of magnetic resonance imaging in determining a treatment regimen. Am J Sports Med 2003;31(2):261.
- Robinson JR et al: The posteromedial corner revisited. An anatomical description of the passive restraining structures of the medial aspect of the human knee. J Bone Joint Surg B 2004;86(5):674.
- Sawant M et al: Valgus knee injuries: evaluation and documentation using a simple technique of stress radiography. Knee 2004; 11(1):25.
- Wilson TC et al: Medial collateral ligament utibiar injuries: indication for acute repair. Orthopedics 2004;27(4):389.
Clinical picture[edit | edit code]
Injuries to the fibular collateral ligament and posterior non-external ligamentous apparatus are relatively rare and are almost always combined with injury to other ligaments, so they are often undetected. The doctor should be alert to symptoms such as pain in the outer and posterior parts of the joint and ecchymosis.
History and complaints[edit | edit code]
The most common symptom of acute peroneal collateral ligament injury is pain in the outer part of the joint. Instability in the outer and posteroexternal sections can be expressed in different ways and depends on the severity of the injury, the patient’s activity, the condition of all joints of the limb and concomitant injuries of the knee joint. For example, in a sedentary person with minimal joint instability and an initial X-shaped curvature of the legs, symptoms may be subtle or absent. Conversely, when instability is combined with O-shaped curvature and hyperextension of the knee joints in a physically very active patient, the symptoms will be very pronounced. Such patients complain of pain in the outer part of the knee joint and a feeling that the leg is turning outward. Symptoms occur during everyday activities, such as walking at a normal speed.
Physical examination[edit | edit code]
Injuries to the fibular collateral ligament and the ligamentous apparatus of the posterolateral section are often combined with injuries to other ligaments of the knee joint. To identify these concomitant injuries, the joint is examined especially carefully. In addition, it is necessary to pay due attention to the diagnosis of damage to blood vessels and nerves, especially the peroneal nerve - its injury accompanies injury to the ligamentous apparatus of the posterolateral part of the knee joint in 12-29% of cases.
The integrity of the fibular collateral ligament is assessed using the adduction test with the knee joint fully extended and flexed at an angle of 30°. The initial width of the joint space in the outer part of the joint can be different; the opposite leg serves as a guide. On average, the angle of divergence of the articular surfaces is 7°. With an isolated injury to the fibular collateral ligament, weakness of the ligamentous apparatus is noted when the knee is flexed to 30°, but the joint should be stable when fully extended. This effect occurs due to the action of intact cruciate ligaments.
It is important to know that a significant injury to the posterolateral ligaments of the knee joint may not be accompanied by a pronounced divergence of the articular surfaces during the adduction test. To detect weakness of the posteroexternal ligaments, an additional test is performed: with the patient lying on his stomach, both legs are turned outward and the angle between the thigh and foot is assessed. The test is carried out with knees bent at 30° and 90°; A difference of 5° or more with the healthy leg is considered significant.
Radiation diagnostics[edit | edit code]
If a serious injury to the knee joint is suspected, a complete x-ray examination is required. Radiographs look for a fracture (including Segon's fracture; see radiology for anterior cruciate ligament injuries), articular mouse, avulsion of the head of the fibula, and luxation of the patella. With chronic posterolateral instability, degenerative changes are often found in the outer part of the joint. Possible narrowing of the joint space with the formation of osteophytes and subchondral sclerosis.
The amount of discrepancy between the articular surfaces can be determined using functional radiography.
Damage to the fibular collateral ligament and posterolateral ligamentous apparatus can often be detected only with MRI. It has already been said that these injuries often go unnoticed during the initial examination, but are obvious on MRI. MRI is of particular value when fear of pain and the patient’s resistance to the doctor’s manipulations prevent an examination.
Diagnostic tests[edit | edit code]
- Reverse test of changing the lateral support point. The test begins with the knee bent at a right angle. By straightening the knee, the doctor turns the shin outward and abducts it. At the moment of reduction of the tibia from the position of posterior subluxation, a noticeable shift occurs.
- Test with external rotation and hyperextension. The patient lies on his back with his legs fully extended. The leg is lifted by the toes. If the quadriceps muscle is sufficiently relaxed, hyperextension in the knee joint is detected, the leg bends inward and the tibial tuberosity turns outward.
- Rear drawer symptom. The symptom of the posterior drawer is determined according to the standard method when the lower leg is rotated inward and outward, as well as in a straight position. In case of injury to the ligaments of the posterolateral section, the severity of the symptom will be greatest when the tibia is rotated outward.
- Examination under anesthesia. The examination under anesthesia allows the patient to relax, which is especially important immediately after an injury. In case of multiple ligament injuries, the examination can be performed under anesthesia before surgery - such an examination is often more informative due to the absence of protective muscle tension.
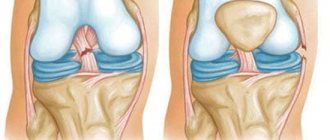
ANATOMY
Ligaments are strong structures of connective tissue that connect bones to each other. The knee joint is strengthened by two collateral (side) ligaments, which prevent excessive abduction and adduction of the tibia. The medial collateral ligament is located on the inner surface of the knee joint, that is, on the side facing the other knee joint. The lateral collateral ligament is located on the outside of the knee joint. Excessive stretching of these ligaments as a result of injury can result in their rupture. The tear line can be located anywhere in the ligament, both in the center of the ligament and at the place where it attaches to the bones. With significant trauma, combined damage to the collateral and intra-articular ligaments of the knee joint can occur.
Most often in clinical practice, a combination of rupture of the medial collateral and anterior cruciate ligaments is observed. The anterior cruciate ligament is located inside the knee joint, in its central part, and its function is to limit the anterior movement of the tibia relative to the femur. The incidence of medial collateral ligament rupture is higher than that of the lateral collateral ligament, but the likelihood of developing knee instability is higher with the latter type of traumatic injury. One reason for the high incidence of joint instability with lateral collateral ligament rupture is that the medial portion of the tibial plateau has a deeper depression. On the contrary, on the side of the lateral collateral ligament, the tibial plateau has a flat surface, and therefore the amplitude of bone movement in this part of the joint is higher.
The force that causes a rupture of the collateral ligament inevitably leads to damage to the soft tissue near the knee joint. As a result, bruising occurs and traumatic swelling of the joint area develops. Some patients experience damage to intra-articular blood vessels, which causes hemarthrosis - accumulation of blood in the joint cavity. The injury causes pain and stiffness in the joint. Many patients, already in the “acute” period of injury, are worried about instability of the joint: the leg twists if the patient transfers body weight to it. Chronic instability of the knee joint as a result of damage to the collateral ligaments is a fairly common pathology. Instability can occur either as a result of complete disruption of the integrity of the collateral ligament, or due to insufficient function of the ligament due to its incomplete or improper consolidation.
Treatment[edit | edit code]
Conservative treatment[edit | edit code]
As noted, isolated injuries to the fibular collateral ligament are rare. In the case of an isolated incomplete rupture, good results are achieved by immobilization of the knee joint for 2-4 weeks followed by strengthening of the quadriceps muscle. With a complete rupture, the results of conservative treatment are worse. Old ruptures and posterolateral instability of unknown etiology are especially difficult to treat.
Surgical treatment[edit | edit code]
So, when developing a treatment plan, you almost always have to take into account injuries to other ligaments. It is advisable to identify injuries to the fibular collateral ligament and posteroexternal ligamentous apparatus immediately, since the best results are achieved by early restoration of the ligaments - in the first few weeks. If necessary, reinforce the tendon suture.
In chronic posterolateral instability, more complex reconstructive surgery is often necessary to restore static resistance to varus load. The point of maximum stress in the fibular collateral ligament lies between the head of the fibula and the lateral epicondyle of the femur. Therefore, it is not so important what kind of material will be used for reconstruction; the main thing is to strengthen the specified area with a graft.
Special methods[edit | edit code]
To improve results in chronic lateral instability, an external osteotomy of the proximal tibia is sometimes indicated to relieve stress on the lateral knee joint.
Rehabilitation[edit | edit code]
The rate of restoration of knee joint function after reconstruction of the posterolateral ligament apparatus depends on whether the cruciate ligaments were damaged. The affected leg should not be weight-bearing for 6 weeks, and protective orthotic devices should be used for at least 3 months.
DIAGNOSTICS
A physical examination (examination, palpation, study of lower limb mobility) allows the doctor to make a presumptive diagnosis of collateral ligament rupture. Physical examination is a valuable diagnostic method, allowing the identification of intra-articular or periarticular ligament rupture in most patients. In the acute period of injury, physical examination is difficult due to severe pain and swelling of the knee joint. In these cases, rest for 5-7 days is prescribed for the injured limb, analgesic medications, and cold (ice packs) on the area of the damaged joint. During this time, the pain subsides and the swelling decreases, which makes it possible to conduct a full physical examination of the knee joint.
X-rays of the knee joint are performed to exclude possible bone fractures due to injury to the knee joint. In order to diagnose a collateral ligament rupture in the presence of symptoms of instability, functional (stress) radiography is necessary. In this case, an x-ray of the joint is taken when the radiologist's assistant moves the patient's lower leg to the side (medially or laterally). The diagnosis is confirmed if widening of the joint space is noted on the side of the collateral ligament rupture. If combined damage to periarticular and intraarticular ligaments, menisci or articular cartilage is suspected, magnetic resonance imaging is indicated. In this case, the image of the knee joint takes the form of a series of longitudinal and transverse sections, which are obtained as a result of digital processing of signals obtained using electromagnetic waves. Magnetic resonance imaging is especially the “gold” standard for diagnosing damage to the soft tissue structures of the knee joint (cartilage, ligaments, tendons). This completely safe and painless research method can be especially useful if the doctor has doubts about the presence of damage to the structures of the knee joint.
Read also[edit | edit code]
- Supplements for ligaments and joints Glucosamine sulfate
- Chondroitin sulfate
- Collagen
- Anterior cruciate ligament rupture
- Chondromalacia patella: symptoms and treatment
Brief Anatomy of the Knee Joint
The joint is formed by 3 bones: the distal epiphysis of the femur, the proximal epiphysis of the tibia, between which are the lateral and medial menisci, and the patella. There are two groups of ligaments:
1. Extracapsular (located outside the joint cavity):
- tibial or internal collateral;
- fibular or external collateral;
- patellar ligament.
2. Intracapsular (located inside the joint cavity):
- anterior cruciate;
- posterior cruciate.