Arthrosis of the foot is a special case of manifestation of arthrosis of the joints with all the characteristics of this unpleasant disease.
Being a consequence of disruption of the metabolic and circulatory processes of cartilage tissue, it leads to the gradual destruction of articular cartilage.
A.
appearance of the foot with arthrosis of the first metatarsophalangeal joint, b.
X-ray of the foot For a person, as an upright creature, the health of the foot is the health of the entire musculoskeletal system.
Suffice it to remember that flat feet, not compensated in time by special orthopedic means, can lead to an increase in the load on higher-lying joints, poor posture, and even contribute to the formation of an intervertebral hernia.
Advanced arthrosis can cause no less trouble, completely depriving a person of the ability to move normally and live a full life without pain.
What joints are affected by arthrosis of the feet?
- metatarsal bones of the foot;
- phalanges of the toes;
- tarsal joints;
- heel bone.
Radiographs show arthrosis of the ankle joint.
You should know!
Most often, the disease affects the joint of the big toe, so patients can notice a characteristic “nomad gait” when, when moving, the main burden is transferred to the outer part of the foot.
Treatment of foot joints using MBST therapy
An effective innovative technique of MBST therapy will help you completely get rid of arthrosis of the foot. This type of treatment starts the metabolic process, the cells begin to recover quickly. The exact cause of the disease is eliminated, while the patient feels a significant improvement in well-being, and the unpleasant symptoms of pain and inflammation go away.
The affected area of the foot is influenced by a special magnetic resonance field. It sends signals that trigger the regeneration process. In this case, the progression of the disease stops, and the active recovery process begins. At the moment, MBST therapy is the most effective and fastest treatment method. After 10 sessions the patient feels improvements. Treatment of arthrosis of the feet using the MBST method allows you to maintain the positive effect for more than 5 years after completing the course.
Moscow, metro station Dubrovka, st. Sharikopodshipnikovskaya, 6/14
| Loading map... |
Risk factors
Osteoarthritis of the foot is a multifactorial disease.
Among the complex of various reasons we can highlight:
- genetic predisposition;
- congenital or acquired deformation of the foot (anomalies in the structure of the limbs, flat feet, unevenly developed limbs);
- regular increased loads on the foot area (especially stationary loads, for example, standing work);
- disruptions in the functioning of the hormonal system (thyroid disease, diabetes, changes in the female body during menopause, etc.);
- regular injuries and microtraumas (typical for professional athletes, ballerinas);
- frequent hypothermia;
- excess body weight;
- wearing uncomfortable shoes (leads to improper redistribution of the load);
- age-related changes.
You should know!
The main risk group is women aged 40 years and older, especially during menopause.
At this time, sudden hormonal changes in the female body can lead to problems with the musculoskeletal system, including arthrosis.
Anyone at risk needs constant monitoring. For this you can use the modern equipment of City Clinical Hospital No. 17. Orthopedic doctor A.S. Petrosyan. will help you diagnose the problem at the earliest stages.
Treatment methods for arthrosis
Treatment of arthrosis is aimed at eliminating the causes that caused the development of arthrosis, eliminating inflammatory changes, restoring lost functions and metabolism in the joints.
The specialists of JSC “Family Doctor” have extensive experience in diagnosing and treating arthrosis. Professional training, modern equipment and our own laboratory allow our orthopedic doctors to make an accurate diagnosis and develop effective treatment tactics for the disease.
Treatment of arthrosis is usually carried out on an outpatient basis. In some cases, you may be offered inpatient treatment for arthrosis.
Conservative treatment
Conservative treatment of arthrosis is complex, including the use of anti-inflammatory and painkillers, as well as physiotherapeutic procedures.
Specialist consultation
General symptoms of arthrosis
- freezing feet (a symptom of poor circulation in the lower extremities);
- “crunching” while driving;
- “ache” due to the weather;
- discomfort and limited joint mobility when walking;
- aching pain, which can be replaced by sharp pain;
- swelling and hyperemia around the inflamed joint;
- painful calluses in areas of primary stress;
- Heberden's nodes (tumors the size of a pea at the level of the interphalangeal joints of the foot; can periodically rupture);
- deformation and destruction of joints (especially the thumb).
This is a common set of symptoms. The full picture of arthrosis can only be described taking into account one or another stage of the disease.
Symptoms of arthrosis
Manifestations of arthrosis begin with pain and crunching in the joints when moving. Subsequently, swelling appears and joint pain intensifies. It becomes difficult to move quickly, climb stairs, or lift weights.
Similar symptoms are characteristic of arthritis. However, arthritis is characterized by inflammatory processes in the joint. With arthrosis, inflammation does not occur from the onset of the disease and can be intermittent, and destructive processes in articular cartilage are caused by metabolic disorders.
Joint pain
The pain can be severe if the movement is preceded by a long stay at rest; after some time after the start of the movement, the pain subsides.
Edema
The affected joint may swell.
Decreased range of motion in a joint
The affected joint loses mobility. Movements in the joint are no longer free, and the possible range of motion in the joint is reduced. Trying to maintain the same range of motion causes pain.
Joint deformity
At a late stage of the disease, deformation of the joint occurs, the joint almost completely loses mobility.
Stages of damage
1st stage. The feet often react to changes in weather with aching joints; joint mobility is impaired, aching pain appears. In the absence of stress, it can be asymptomatic for a long time.
2nd stage . Pain occurs more often, intensifying as the disease progresses. The first metatarsophalangeal joint becomes inflamed and increases in size, which leaves its mark on the gait and tightens the requirements for wearing shoes.
3rd stage. Pain becomes a constant companion. The level of deformity of the joint limits the movement of the foot. The thumb curls and moves down. Degenerative processes spread to soft tissue and bone, depriving the patient of the ability to move freely.
Requirements for sports shoes.
Particular attention should be paid to shoes. Shoes should be well chosen in both length and width. There should be a distance of 1 cm between the tip of the longest toe and the toe of the shoe. Poorly fitting shoes can permanently damage the foot. Tight shoes create painful calluses on both sides of the foot. Choose a flexible, stretchy but firm sole and soft upper. Heavy leather boots are not the best option for you. Laces and small buckles can make it difficult to put on shoes, so it is better to replace them with elastic inserts. You need sports shoes or sneakers with thick, well-cushioned soles. The sole should be 2-3 cm thick or have a thicker flat heel. The leather or material from which the shoes are made should not be very hard. Two instep supports should be inserted inside to support the longitudinal and transverse feet. The fastener of sports shoes should make it possible to grasp the feet without interfering with blood circulation. Sports shoes with Velcro are comfortable and easy to put on.
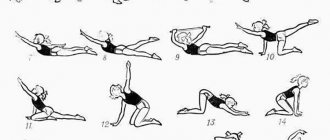
Exercises during an exacerbation
During the period of exacerbation, when there is pain at rest, swelling, redness of the joint, it is necessary to reduce physical activity. Reduce the amount of daily workload for yourself. Under no circumstances should movement be carried out “through force.” Do not perform movements that cause acute pain.
Exercises during remission
During the period of remission, there is no pain in the joint at rest, but there may be discomfort during movements of large amplitude or mild pain after physical activity. During this period, it is necessary to return to the muscles their strength, which they lost during the period of exacerbation. This can be done by performing the exercises slowly, gradually increasing the number of repetitions. While performing these exercises, you should feel your muscles working hard, so some discomfort may be associated with the exercises. However, these exercises should not cause severe joint pain or joint swelling after performing them. If you easily perform the exercise once, then repeat two or three times, gradually increasing the number of repetitions.
Diagnostics
An external examination and conversation with the patient is sufficient to make a primary diagnosis.
However, in order to exclude similar pathologies (grade II flat feet, gout, heel spur, rheumatoid arthritis, etc.), as well as to determine the level of damage, additional studies should be performed:
- radiography (records degenerative changes in cartilage tissue and the stage of their development);
- laboratory tests (check for the presence of rheumatoid changes);
- magnetic resonance or computed tomography (if necessary).
Causes of deforming arthrosis
The main cause of osteoarthritis is age-related changes associated with hormonal changes in the body, a decrease in the strength of cartilage and bone tissue, a slowdown in metabolism and a deterioration in blood microcirculation due to wear and tear of the heart and blood vessels. However, a number of causes of deforming arthrosis can provoke the disease at a young age:
- physical or emotional stress;
- inconveniently equipped workplace;
- injury, infection or surgery;
- hypothermia (including due to drafts);
- abuse of alcohol and tobacco products;
- depression and other changes in metabolic processes;
- overweight;
- specifics of professional activity (work in hot shops, with vibrating tools or in transport, temperature changes, heavy lifting).
Based on the causes, deforming arthrosis is divided into primary and secondary. Primary osteoarthritis occurs directly under the influence of external or age-related factors. The secondary one is indirect - it is triggered by another disease (for example, diabetes mellitus, rheumatoid arthritis, necrotic pathology in the hip joint, Perthes disease, etc.).
Conservative treatment
Conservative techniques eliminate the main symptoms of arthrosis and activate tissue regenerative processes, namely:
- relieve pain;
- stop inflammatory processes;
- improve blood circulation in the joint area and the entire limb;
- restore cartilage tissue.
Important!
Treatment of multifactorial diseases must be comprehensive, therefore, in the fight against arthrosis of the feet, it is necessary to use several areas at once, including working with the cause (excess weight, hormonal imbalance, bad shoes, etc.).
Conservative techniques include:
- drug treatment of arthrosis using non-hormonal and hormonal (for severe cases) drugs, analgesics, as well as drugs to improve blood circulation and chondroprotectors;
- Exercise therapy and massage (useful in the initial stages, helping to improve nutrition of damaged areas of the foot);
- a diet low in salt, smoked, pickled and refined foods, enriched with protein and vitamin dishes high in calcium, silicon, zinc, magnesium and other microelements important for the musculoskeletal system;
- physiotherapy such as ultrasound, heat, laser therapy, electrophoresis or magnetic resonance therapy.
Arthrosis of the foot: symptoms and treatment
As mentioned earlier, classical treatment of foot joints is a complex process. It is divided into medicinal treatment and preventive treatment. The medicinal method consists of the following procedures:
1. Treatment of arthrosis of the feet with the use of non-steroidal painkillers. The new generation of drugs makes it possible to achieve not only the prevention of the development of inflammatory processes, but also relieve the patient from uncomfortable pain. These medications show high effectiveness after using them in a course. The dose and duration of administration are determined by the attending physician.
2. If the person has severe pain, they are given a corticosteroid injection. Due to the fact that the medicine contains quite strong substances, the use of this injection is permissible only once every seven days.
3. The most common drug for the treatment of foot joints is a chondroprotector. Its action is aimed at restoring damaged cartilage and protecting it from subsequent deformation.
4. A medicine based on hyaluronic acid is often used to treat degenerative foot disease. Injection injections allow you to increase the motor capabilities of the leg joints and reduce pressure on them.
5. As a preventive treatment for arthrosis of the feet, a special ointment and cream can be prescribed, which have a beneficial effect on the feet.
Preventive treatment of foot arthrosis is also widely used. It is worth noting that all of the following methods can be used both as a prophylactic to prevent the occurrence of this disease, and in combination with drug treatment of already progressing arthrosis of the foot:
1. Application of the so-called plaster “boot”. It is prescribed to a patient in the presence of a severe stage of development of the disease, when it is necessary to eliminate it as soon as possible.
2. Using an orthopedic insole or arch support. They are aimed at increasing blood flow in the joints of the legs. In turn, they promote tissue metabolism.
3. Regular foot massage. Its use is permissible at almost all stages of arthrosis. However, it is recommended to refrain from this procedure during periods of acute pain.
4. To increase the effectiveness of drug treatment, the patient may be prescribed laser and magnetic therapy.
5. The use of therapeutic mud allows the leg joints to receive the necessary beneficial vitamins for their normal functioning, as well as relieve excessive stress during physical activity.
6. Surgical intervention is a procedure that is prescribed to a patient who is in the last stage of arthrosis of the foot. If there is no desired result from the use of alternative methods and medicines, the patient will require surgery.
Main diagnostic method
The main diagnostic method is x-ray examination, which shows a narrowing of the joint space, thickening of the articular surfaces, sharpening of the intercondylar tubercles, and marginal bone growths (osteophytes). At stages 3-4 of arthrosis, the joint space is practically absent (photo* below).
To clarify the diagnosis, ultrasound and MRI (magnetic resonance imaging) of the knee joints are performed according to indications.
Does varicose veins of the lower extremities affect the manifestations of osteoarthritis of the knee joints?
Osteoarthritis (OA) is the most common joint disease, occurring in approximately 11–13% of the world's population, more often in women [1]. Thus, at the age of 50–59 years, OA of the supporting joints is detected in 16% of Russian women [2]. Chronic venous diseases are also widespread in the population. According to the results of the Russian DEVA study, which examined 3,788 women aged 18 to 65 years, 21.7% of participants had varicose veins (VD) of the lower extremities [3]. There is also evidence of a frequent combination of these diseases [4–6]. It is unclear whether this combination is a coincidence due to the widespread prevalence of both diseases in the population or the commonality of risk factors (age, female gender, obesity, increased load on the lower extremities, etc.) [3, 7–10], or whether the two diseases have common developmental mechanisms, for example, connective tissue dysplasia [11–13]. At the same time, the question of their possible mutual influence on each other is of practical interest, in particular, whether concomitant pathology of the veins of the lower extremities contributes to a more severe course of OA. This determined the purpose of this study - to identify risk factors for the development of VV of the lower extremities in patients with OA of the knee joints and to evaluate the possible impact of VV of the lower extremities on the clinical manifestations of gonarthrosis.
Materials and research methods
The study was conducted at the Department of Preventive and Family Medicine of the Ural State Medical University (USMU) of the Ministry of Health of Russia on the basis of the city rheumatology center of the city clinical hospital No. 40. The study was approved by the ethics committee of the USMU. Before inclusion in the study, all patients signed informed consent.
Selection of patients for the study
Patients were recruited at a rheumatologist's appointment. Criteria for inclusion in the study:
- female;
- age 40–60 years inclusive;
- the presence of OA of the knee joints in accordance with the clinical, laboratory and radiological criteria of the American College of Rheumatology (ACR) 1986 [14].
Criteria for non-inclusion in the study:
- indications of severe injuries to the lower extremities;
- history of operations on the joints of the lower extremities;
- previous inflammatory joint diseases;
- clinical signs of hip OA;
- the presence of spinal diseases accompanied by signs of radiculopathy;
- neuropathic pain in the lower extremities;
- history of deep vein thrombosis of the lower extremities;
- congenital anomalies of the veins of the lower extremities.
Thus, the study did not include patients with possible secondary OA of the knee joints and women who had diseases that could complicate the assessment of the clinical manifestations of OA of the knee joints and VVD of the veins of the lower extremities. A total of 85 patients were included in the study.
Research methods
All patients underwent a clinical examination, which included collection of complaints and an objective examination with an emphasis on symptoms of OA and the condition of the veins of the lower extremities, and an assessment of possible risk factors for VD. The severity of OA was assessed using the Lequesne index (M. Lequesne) [15]. All of them underwent radiography of the knee joints in two projections, assessed according to I. Kellgren & I. Lawrence (1957). The diagnosis of VD was made in accordance with the international CEAP classification [16], according to which saphenous veins of the lower extremities with a diameter of more than 3 mm in a standing position, having a nodular and/or tortuous appearance, were regarded as varicose veins (varicose veins), which corresponds to clinical class C2. Edema of the lower extremities corresponds to C3 clinical class. Trophic disorders of the skin and subcutaneous tissue of the lower extremities were considered to be the presence of hyperpigmentation of the legs and/or signs of venous eczema, lipodermatosclerosis and/or white skin atrophy (class C4). The presence of healed or open venous ulcers corresponds to class C5–C6. Chronic venous insufficiency is diagnosed in the presence of clinical manifestations of C3–C6 [16].
All participants were also examined to identify signs of connective tissue dysplasia (CTD). The criteria for the severity of DST were taken as a basis by T. Yu. Smolnova (2003) [17], from which, for greater confidence, we selected for analysis the following manifestations of DST: ventral hernias, splanchptosis, as well as repeated dislocations of one joint or dislocations of two or more different history of joints. The choice of these signs of DST was due to their vivid clinical picture and relatively simple identification according to anamnesis or physical examination. To identify splanchptosis, questions were asked about the presence of a history of prolapse of the uterus, kidneys, and organs of the gastrointestinal tract, while the prolapse of at least one of these organs was regarded as splanchptosis. Joint hypermobility was also assessed using the Beighton test [11].
Statistical processing was carried out using the Statistica 6 program. To describe quantitative normally distributed data, the mean value of the indicator and standard deviation were used, for quantitative non-normally distributed characteristics - the median and interquartile range. Comparison of quantitative characteristics under the condition of normal distribution was carried out using the Student's test. Quantitative non-normally distributed traits were assessed using the Mann–Whitney test. Qualitative binary variables were compared using two-sided Fisher's exact tests. Differences were considered statistically significant at p < 0.05.
results
Among 85 patients with OA of the knee joints, 37 (43%) people were diagnosed with VAD of the lower extremities (class C2 according to the CEAP criteria); they formed the main group. Among them, venous edema of the lower extremities (class C3) was present in 17 participants (46%), trophic changes in the skin and subcutaneous tissues (class C4) in 7 people (19%), there were no patients with open or closed venous ulcers in the study. In total, there were 24 (65%) patients with signs of chronic venous insufficiency (class C3–C6). 4 people (10%) underwent surgery for VD of the lower extremities. The remaining 48 (57%) people had no signs of VD of the lower extremities and formed the control group.
The main and control groups did not differ in age (53.3 ± 6.3 and 53.8 ± 4.4 years, respectively, p = 0.69), body mass index (BMI) (33 ± 7.4 and 32. 2 ± 6.3 kg/m2, respectively, p = 0.58), by the frequency of obesity (BMI ≥ 30 kg/m2) (54% and 65%, respectively, p = 0.4). There were also no differences in the proportion of women undergoing menopause (81% of the main and 83% of the control groups, p = 0.8), in the duration of menopause: in the main group the median was 5 years (lower quartile 3, upper 9 years), and in the control group 7 years (lower quartile 3, upper 10 years), p = 0.58.
When analyzing the risk factors for VD of the lower extremities, it was revealed that heredity burdened with VD of the lower extremities was registered more often in women of the main group than in the control group (relative risk 1.9, 95% CI 1.2–3.1). There were no differences in other possible risk factors for VD of the lower extremities (Table).
We also compared the frequency of various signs of CTD in the compared groups (Table). It turned out that patients with OA who also had venous pathology had a history of prolapse of one or more organs (kidneys, uterus, gastrointestinal tract) almost twice as often as compared with women in the control group (relative risk 1.65, 95% CI 1.0–2.7). They were also more likely to have multiple dislocations of one or more joints (relative risk 1.8, 95% CI 1.2–2.9). Joint hypermobility at the time of examination did not differ in both groups.
To study the possible influence of WB on the manifestations of knee OA, we compared complaints, age of onset of the disease, frequency of exacerbations and objective signs of OA in both groups, but differences, including stiffness, crepitus, joint instability, the presence of synovitis, bursitis, joint space tenderness and impairment functions have not been identified. There were no differences between the groups in the X-ray examination: in the main group, stage 2 according to I. Kellgren & I. Lawrence was diagnosed in 9 (30%) versus 18 (38%) in the control group (p = 0.6), 3 stage 2 - in 2 (7%) versus 2 (4%), respectively (p = 0.6). The Lequesne OA severity index was higher in patients with OA and VD of the lower extremities: median 10 points (lower quartile 7.5, upper quartile 15.5) than in patients with isolated OA - median 7 points (lower quartile 3, upper 12 ), although statistically insignificant - p = 0.4.
Discussion
In recent years, work has increasingly raised the question of the need for a personal approach to predicting the course of knee OA, taking into account all concomitant conditions and diseases that could affect the progression, severity of manifestations or response to OA therapy. Thus, the first attempts are being made to create a personal calculator to calculate the risk of progression of knee OA by analogy with the SCORE scales for assessing the risk of developing cardiovascular events or FRAX osteoporotic fractures [18]. We hypothesized that, despite the commonality of some risk factors for OA of the knee joints and VVD of the veins of the lower extremities, the latter may more often develop in patients with OA who have additional risk factors specific to it, and also that damage to the veins of the lower extremities may aggravate the manifestations and severity of the articular process.
Our study showed that risk factors common to the two diseases, such as lifting weights of more than 10 kg, standing for long periods of time, and professional sports, were found with equal frequency in patients with OA, regardless of the presence or absence of VD. It would be logical to assume a higher BMI in the group of women who had combined pathology of the joints and veins, but this was also not found. There is probably no direct relationship between the degree of obesity and the number of diseases associated with it.
The incidence of risk factors specific to chronic venous disease, such as pregnancy, constipation, prolonged sitting, use of menopausal hormone replacement therapy, and wearing high heels, also did not differ between groups. Patients who had a combination of OA with venous disease only more often indicated the presence of VD in relatives. Interestingly, the Russian research program FACT, which covered 8840 patients with chronic venous insufficiency (CVI) and also revealed a similar relationship, showed that the risk of developing CVI in both women and men is more influenced by the dilation of the veins in the mother than in the mother. father [10]. Of particular interest is another risk factor for both diseases—DST. Today, external and visceral signs of hereditary connective tissue disorders in many organs and organ systems have been clearly described [11–13], but there are no uniform approaches to assessing the severity of CTD. Since our study was not prospective and the goal of our work was not to study DST as a risk factor for OA and VD, we limited ourselves to comparing groups according to the three most striking features: a history of ventral hernias, splanchptosis, repeated dislocations of one or dislocations of two or more joints. All these signs, according to the criteria of T. Yu. Smolnova, relate to severe manifestations of DST, gain a higher number of points and are interpreted as “severe manifestations and conditions leading to surgical interventions or having indications for them, as well as changes in anatomical relationships leading to disruption organ functions" [17]. In our study, in the group with a combination of OA of the knee joints and VAD of the lower extremities, repeated dislocations and subluxations of the joints occurred twice as often as in the group with isolated OA. Patients with OA and venous involvement were also more likely to have a history of prolapse of the uterus, kidneys, or gastrointestinal tract organs. At the same time, the Beighton test, which characterizes joint hypermobility at the time of the study, did not differ between groups, although the score was slightly higher in patients with OA and VD (2 points versus 0 in the group of isolated OA), but not statistically significant (p = 0.53) . This seems natural, since joint hypermobility has the lowest diagnostic sensitivity among the external signs of hereditary connective tissue disorders and decreases with age [11]. Thus, in our group, patients with a combination of OA of the knee joints and VD of the lower extremities had a history of more manifestations of dysplasia (splanchptosis, repeated dislocations of the joints) compared to patients with OA of the knee joints without venous involvement.
According to our data, the presence of VB of the lower extremities did not affect the clinical manifestations of OA of the knee joints. The Lequesne index was higher in the group with a combination of OA of the knee joints and VAP of the lower extremities, but the difference did not reach statistical significance.
The assumption that lower extremity venous disease may aggravate the manifestations of knee OA seems logical. Thus, previously, in a group of patients with OA of the knee joints (158 people aged 40 to 78 years, 96.8% women), it was shown that the combination of OA with VVD of the lower extremities or postthrombophlebitic syndrome is accompanied by an increase in the intensity of pain in the joints at rest and during movement (according to VAS) and a decrease in functional activity according to the Lequesne and WOMAC indices [5]. R. M. Nagibin et al. found that patients with a combination of gonarthrosis and venous hypertension in the lower extremities have a higher intensity of night pain and functional failure according to WOMAC [19]. However, there are other data. Thus, in the work of E. A. Shcheglov et al. when comparing a group of patients with OA of the knee joints and signs of CVI against the background of VD of the lower extremities (40 patients, average age 54.3 ± 7.9 years, 85% women) with a group of patients with OA of the knee joints without manifestations of CVI (40 people, average age 58.1 ± 8.2 years, 80% women) it was shown that patients with venous lesions noted increased pain according to VAS only in the evening hours; there were no differences between groups in the intensity of pain in the morning, as well as in the Lequesne index and WOMAC was obtained [20]. Obviously, the differences in the results of the above studies may be associated with the age and gender composition of the participants, the assigned tasks, as well as the use of different classification approaches and diagnostic methods. Thus, some researchers assessed the effect of VV with signs of CVI, others - the effect of chronic diseases of the veins of the lower extremities on the course of OA of the knee joints. In addition, it is not always clear what researchers meant by the term CVI - the presence of swelling of the legs or severe changes in tissue trophism, venous ulcers. In our work, the lack of convincing differences between groups in the severity of OA of the knee joints (Lequesne index) may be due to the fact that patients with VB did not have severe manifestations of CVI (only 19% of participants had changes in the skin and subcutaneous tissue, and open venous ulcers or there were no healed ones) and moderate manifestations of CVI did not affect the severity of OA.
Our study has limitations. The design of a single-stage study did not allow us to provide clinical characteristics of osteoarthritis over time, and a retrospective analysis of signs of connective tissue dysplasia made it possible to study only a narrow range of its manifestations. We did not study quality of life, and the study did not include patients with severe manifestations of CVI.
Thus, heredity aggravated by VD of the lower extremities and connective tissue dysplasia may be risk factors for the development of VD of the lower extremities in patients with OA of the knee joints. The possible influence of connective tissue dysplasia on the simultaneous development of OA and VD of the lower extremities requires more in-depth study in specially designed studies. It cannot be excluded that the severity of OA of the knee joints is influenced not so much by the VB of the lower extremities as by the degree of CVI.
Literature
- Alekseeva L. I. Modern treatment of osteoarthritis // Pharmateka. 2012. S1–12. pp. 22–27.
- Danchikova A. M., Batudaeva T. I., Menshikova L. V. Prevalence of osteoarthritis of large joints among residents of the Republic of Buryatia // Bulletin of the All-Russian Scientific Center of the Siberian Branch of the Russian Academy of Medical Sciences. 2011. No. 1 (77). pp. 205–208.
- Zolotukhin I. A. Chronic venous diseases in women: results of the Russian screening study DEVA // Consilium Medicum. Applications. 2008. No. 8. pp. 128–131.
- Nasonova V. A. Osteoarthrosis is a problem of multimorbidity // Consilium Medicum. 2009. No. 2. P. 5–7.
- Salikhov I.G., Lapshina S.A., Myasoutova L.I., Kirillova E.R., Mukhina R.G. Osteoarthrosis and diseases of the peripheral veins of the lower extremities: features of combined pathology // Therapeutic archive. 2010. No. 5. P. 58–60.
- Shcheglov E. A., Vezikova N. N., Kartsova I. V., Rybakov V. I., Kheifets I. V. Ultrasound diagnostic algorithm for the combination of varicose veins and osteoarthritis of the knee joints // Bulletin of experimental and clinical surgery. 2012. No. 5 (1). pp. 14–19.
- Lesnyak O. M. et al. Osteoarthrosis of large joints of the lower extremities. A guide for primary care physicians. M.: GEOTAR-Media, 2021. 144 p.
- Zolotukhin I. A. Risk factors for chronic venous insufficiency of the lower extremities and the possibility of its drug treatment // Consilium Medicum, Surgery. 2006. T. 8. No. 1. P. 40–43.
- Savelyev V.S., Kirienko A.I., Bogachev V.Yu. Chronic venous diseases in the Russian Federation. Results of the international research program VEINCONSULT // Phlebology. 2010. No. 3. pp. 9–12.
- Bogachev V. Yu., Zolotukhin I. A., Kuznetsov A. N. Chronic diseases of the veins of the lower extremities: modern view of pathogenesis, treatment, prevention // Phlebology. 2008. No. 1. P. 43–50.
- Shostak N. A. Pravdyuk N. G. Kotlyarova L. A. Hypermobility syndrome: an internist’s view // Modern rheumatology. 2012. No. 1. pp. 24–28.
- Tyurin A.V., Davletshin R.A. On the pathogenesis of osteoarthritis and connective tissue dysplasia // Medical Bulletin of Bashkortostan. 2013. No. 8 (4). pp. 80–83.
- Viktorova I.A. Konshu N.V. Osteoarthrosis in patients with familial joint hypermobility: stratification of the risk of occurrence and type of progression // Medical Bulletin of the North Caucasus. 2014. No. 4 (9). pp. 310–314.
- Altman R., Asch E., Bloch D. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association // Arthritis Rheum. 1986. Vol. 29. 8. P. 1039–1049.
- Leguesne M., Mery C. The algofunctional indicators for hip and knee osteoarthritis // J Reumatol. 1997. No. 24. R. 779–81.
- Russian clinical recommendations for the diagnosis and treatment of chronic venous diseases // Phlebology. 2013. No. 2. P. 8–17.
- Smolnova T. Yu., Savelyev S. V., Yakovleva N. I., Grishina V. L., Baranov V. M. The phenomenon of generalized cytopenia in patients with prolapse and prolapse of the internal genital organs - as a phenotypic manifestation of connective tissue dysplasia syndrome / / Medical Bulletin of the North Caucasus. 2008. No. 2. P. 44–48.
- Losina E., Klara K., Michl GL, Collins JE, Katz JN Development and feasibility of a personalized, interactive risk calculator for knee osteoarthritis // BMC Musculoskelet Disord. 2015, Oct 22. No. 16. R. 312.
- Nagibin R. M., Kozlova O. G. The influence of physical exercise on the course of gonarthrosis in patients with concomitant venous hypertension / Materials of the 4th National Congress of Therapists. M., 2009. P. 308.
- Shcheglov E. A., Vezikova N. N. Features of the clinical picture in patients with osteoarthritis of the knee joints and combined lesions of the veins of the lower extremities // Modern problems of science and education. 2012. No. 1.
E. V. Zubareva*, 1 O. M. Lesnyak**, Doctor of Medical Sciences, Professor
* MAU City Clinical Hospital No. 40, Ekaterinburg ** Federal State Budgetary Educational Institution of Higher Education USMU Ministry of Health of the Russian Federation, Ekaterinburg
1 Contact information
Diagnosis of coxarthrosis
The diagnosis of coxarthrosis is made based on a number of criteria developed by the American College of Rheumatology (ACR) in 1990. To make a diagnosis, the presence of pain in the hip joint and two clinical and radiological signs out of the following three are necessary: ESR <20 mm/h; osteophytes of the femoral head or acetabulum; narrowing of the joint space.
The photo below shows an x-ray with severe arthrosis of the hip joint.