The process of deciphering survey results
After the radiologist receives the X-ray images, he needs to interpret them and draw up a conclusion.
To decipher the results, there is a special technique called the Hilgenreiner scheme. It contains the following categories:
- acetabular angle;
- Hilgenreiner line;
- the distance between the metaphyseal plates and the Hilgenreiner line, denoted by the letter h;
- the distance from h to the lower contours of the vestibular plate, denoted as d.
The acetabular angle is defined as the area between two planes - the line of epsilon-shaped cartilages and the tangent running along the edge of the glenoid sockets.
Hilgenreiner's line is drawn horizontally through the Y-shaped cartilages along the lower points of the ilium.
Distance h is measured from the Hilgenreiner line to the middle of the metaphyseal plate of the proximal femur. It can be used to track how much the head of the femur is displaced in relation to the socket of the joint.
The d gap shows the lateral displacement of the head compared to the acetabulum.
The diagram makes it possible to represent the joint in a three-dimensional projection. Even at the earliest stages, it makes it possible to detect most pathologies and disorders of joint development.
For greater reliability, the scheme provides for additional indicators - the Calvet and Shenton lines. The first of them connects the upper edge of the femoral neck with the outer edge of the ilium, and normally it should be continuous. If the line is interrupted, this may indicate a lack of integrity of the articular apparatus.
Shenton's line is a continuation of the circumference of the acetabulum, in the form of a projection onto the medial surface of the femoral neck. Its rupture means lateral-proximal displacement of the femur.
How is an X-ray of a child’s hip joint interpreted using the Reinberg scheme?
This image interpretation technique uses the midsacral line, a horizontal line through the apices of the Y-shaped cartilages and the centers of the ossification nuclei in the femoral heads (line A), and a vertical line through the superolateral prominence of the acetabulum (line B) . In addition, determining the normal condition of the joint is associated with the location of the lower edge of the femoral neck - with normal development of the joint, it crosses the lower contour of the groin bone.
An auxiliary line is drawn between line B and the median sacral line, the length of which helps to assess the condition of the joint.
Dysplasia is determined if the proximal end of the femur is above line A and as if outside of plane B.
What is the Ombredan scheme?
In the process of examining the results of radiography, the doctor draws a horizontal line along the synostoses in the image, connecting the pubic and ilium bones. A vertically lowered perpendicular is drawn to the outer edge of the acetabulum of the joint. This perpendicular divides the articular cavity into equal segments, in relation to which the compliance of the anatomy of the joint with normal indicators is assessed.
Normal and deviations in the image of the hip joints
The resulting image of the joint, if it is in a normal state, visualizes the head of the femur located in the glenoid cavity, which has the appearance of a notch. In the center, the head is attached to the surface of the cavity by the round ligament and joint capsule. From above, the head is held in its normal position by the limbus, a cartilaginous plate. The entire articular apparatus is supported externally by the muscular corset of the thigh.
Dysplasia in the image is characterized by a delay in the development of ossification. Ossification nuclei are small in size compared to normal. Dislocation or subluxation can be detected by the lateral and vertical displacement of these nuclei, thanks to the use of Ombredan, Reinberg, and Hilgenreiner schemes.
In what cases are children prescribed x-rays of joint joints?
Responsibility for the health of the child from the first days, in addition to the parents, lies with the neonatologist and pediatrician. These doctors conduct the very first examination in the baby’s life. As for the orthopedist, parents and the child should see him no later than a month after his birth.
However, even before visiting an orthopedist, the parents or pediatrician themselves may suspect dysplasia during the initial examination. This is possible in severe forms of the pathology, if the head of the femur completely protrudes from the acetabulum. If dysplasia does not affect the articular apparatus so severely, only a specialist with appropriate qualifications can determine it.
Signs that should alert parents and pediatricians:
- impaired joint mobility, difficulty spreading the hips, to the point that the child cries when trying to move the leg to the side;
- asymmetry of the inguinal and gluteal folds: on the side where the joint is affected by dysplasia, they are more pronounced;
- shortening of the leg, if the pathology is developed in only one joint;
- clicking symptom: the head of the femur pops out of the socket of the joint with a characteristic sound when the child bends the legs at the knee and hip joints.
Diagnosis of pathology can occur directly in the maternity hospital, while the child is there with the mother after childbirth. Dysplasia can be identified by an orthopedist during the first appointment. In any case, if any of the doctors detects signs of dysplasia in a child, it becomes necessary to visually assess the degree of damage to the joint, its structure, the shape of its components and how they come into contact. For these purposes, the doctor sends the baby for diagnostic examinations.
X-rays of the hip joints in children are not performed in every case. Due to the fact that the procedure involves x-ray exposure of the patient, children under the age of three to four months are not recommended to undergo x-rays at all. An orthopedic surgeon may prescribe preventive measures without x-rays, for example:
- use of soft tires with spreading mechanisms;
- massage of the gluteal muscles;
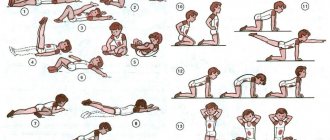
- course of special therapeutic gymnastics.
In each specific case, the doctor decides whether to send the child for an ultrasound of the joint or for an x-ray. Some doctors are guided by the principle “any diagnosis is better than no examination and treatment.” X-rays are advisable if the benefit from the information received outweighs the likely threat to the baby’s health from radiation exposure. Otherwise, the doctor gives the little patient a referral for an ultrasound of the joint.
Reasons for the development of the disease
Cervical dysplasia and pregnancy
Of course, most parents who lead a healthy lifestyle are interested in where the pathology comes from. And the reasons for this can really be very different:
- The main cause of dysplasia is a genetic predisposition, which is transmitted through the mother - in 1/3 of cases.
- The large size of the fetus also affects the formation of the musculoskeletal corset, especially if the child is placed incorrectly in the womb, bones become displaced. However, no matter the size of the baby, its abnormal position in the uterus has a negative impact on the baby’s health.
- The mother's use of medications, as well as exposure to radioactive substances and pesticides, has a detrimental effect on the development of the fetus.
- The presence of kidney disease leads to insufficient development of bones and joints.
- Pronounced toxicosis.
- Uterine tone, which is noted throughout pregnancy.
- Various health problems of a pregnant woman: heart disease, liver disease, anemia, serious metabolic disorders.
- Any infections that the pregnant woman suffered during these 9 months.
- Tight swaddling.
X-ray morphometry
It consists of drawing a horizontal line through both Y-shaped cartilages, then from the highest point of the femoral diaphysis, drawing a line perpendicularly until it intersects with the horizontal line. Normally, the length of this perpendicular (h) is 1-1.5 cm. The distance from the bottom of the acetabulum to the perpendicular (D) is normally also 1-1.5 cm. With dislocation, the distance (h) decreases and (D) increases. A tangent line is drawn from the bottom of the acetabulum to the most peripheral part of the roof of the acetabulum. The resulting angle (a) (acetabular index) usually does not exceed 30°, but in children under 3 months it is very variable (12°-38°). Therefore, this scheme is most suitable for assessing the condition of the hip joint in children older than 3 months.
A line (B) is drawn through the superolateral protrusion of the acetabulum parallel to a line drawn through the middle of the sacral vertebrae. Thus, the joint is divided into four quadrants. With dislocations and dysplasia, the center of ossification is determined in the outer quadrants. In children in the first days of life, the ossification point of the femoral head is absent, therefore, with dysplasia, a displacement of the proximal metaepiphysis outward from the vertical Ombredan-Perkins line is noted. This scheme is convenient for identifying dysplasia in children in the first days of life, especially since it is little affected by errors (small distortions) in placement.
X-ray of the hip joints: the essence of the method
Cervical dysplasia
Classic X-ray examination is based on the ability of specific R-rays to pass through solid objects of different densities with different intensities. Radiation of this type was discovered at the end of the 19th century, and after 15-20 years it began to be used in medical institutions for diagnostic purposes.
The patient is examined using a special device. The patient is placed in the beam projection area, and the image is captured, as if photographing the patient. Instead of photographic film, X-ray film is used, treated with a chemical composition containing silver bromide; instead of a camera, a device with an X-ray tube producing R-rays is used.
The images obtained in this way are highly accurate and informative; bone formations and joints, in particular the hip, are especially well and clearly visible.
Preparing the child and technique of the procedure
There is no need to carry out any specific preparatory measures before taking x-rays of the hip joints. For very young patients, you need to follow a normal sleep and feeding schedule. For children older than a year or a year and a half, you can clearly and generally explain what will happen during an x-ray, tell them that the upcoming procedure is painless and there is no need to be afraid of it.
The child lies on his back during the x-ray. In this case, the patient’s legs should be straight and straight and should not be bent. In newborn babies, the legs move closer to the body and move slightly inward.
If the child’s pelvis is tightly pressed by the cassette to the plane of the couch or table, his movements will not interfere with the recording of the image. The genitals are covered with a protective lead apron to prevent exposure to X-ray radiation.
If there are no contraindications to the use of anesthesia, the procedure can be performed with the young patient under general anesthesia to ensure the accuracy and quality of the images.
Operations for hip dysplasia
Cervical dysplasia grade 1
There are several methods of surgical treatment of hip dysplasia:
Surgeries to restore normal joint biomechanics and increase stability. The purpose of such operations is to preserve the joint and ensure the functionality of the limb on par with a healthy one:
- Triple (double) pelvic osteotomy, method of simultaneous bilateral pelvic osteotomy RL Rooks.
- DARthroplasty – restoration of the dorsal edge (dorsal rim arthroplasty).
- Intertrochanteric osteotomy - used to increase the neck-diaphyseal angle (in some cases, a triple pelvic osteotomy and its variants are sufficient).
Surgeries to relieve pain:
- Myotomy of the pectineus muscle (practically not used due to low effectiveness).
- Denervation of the joint capsule (we do not use this method due to its low effectiveness).
These surgeries may temporarily relieve pain but do not change the course of osteoarthritis. As a rule, after these operations it is necessary to resort to other surgical treatment.
- Resection arthroplasty of the hip joint.
This operation helps relieve the patient of pain for a long time, but cannot fully restore limb function and normal biomechanics. Despite the fact that many dogs walk without limping, muscle atrophy still persists due to the fact that the limb is not fully loaded and the dog tries not to perform certain movements. Small dogs weighing up to 20 kg have a good quality of life. This operation is used as a last resort and is used when other treatment is impossible due to indications or due to financial difficulties of the owner who does not have the means to replace the hip joint.
A separate point worth highlighting is total hip replacement. This operation can fully restore the function of the limb and is used when other methods are ineffective.
Causes
Confirmation of a violation of the primary anlage is evidenced by cases of combination of hip dysplasia with other congenital defects.
As for the second point of view, its supporters consider the cause to be the unfavorable influence of exo- and endogenous factors on the fetus.
This is confirmed by the study of the external environment in industrially polluted areas, where the percentage of dysplasia is much higher.
So, these two theories provide the basis for uncovering the etiology of congenital hip dysplasia.
Typical for hip dysplasia is hypoplasia of the acetabulum: it is small, flat, elongated in length, with varying degrees of increase in the bevel of the arch (beyond 30°).
As a rule, with hip dysplasia, the ossification nuclei of the femoral head appear late and its development is delayed.
The physiological torsion of the proximal end of the femur is disrupted: excessive (more than 10°) rotation (deviation) of the head and neck of the femur occurs anteriorly - antetorsion or, less commonly, backward retroversion with an increase in the neck-shaft angle.
With congenital dysplasia of the hip joint, there is always dysplasia of the muscles, capsule and ligaments.
A feature of dysplasia, in contrast to subluxation or dislocation of the hip, is that the head is always centered in the acetabulum.
At the present stage of medicine, obstetricians, midwives, and visiting nurses must undergo appropriate training in diagnosing congenital defects, especially dysplasia, congenital hip dislocation, torticollis and flat feet.
What causes the development of hip dysplasia?
The causes of the pathology are still debated. Dysplasia can be congenital or develop at an early age, as a result of a violation of the formation of tissues from which the joint subsequently develops. Some cases still occur due to genetic predisposition on the maternal side. Of course, problematic pregnancies can also affect tissue and joint development. From this, the following risk factors are determined:
- maternal toxicosis
- breech presentation of the fetus,
- the fruit is too large, which is why it does not have enough space for range of motion in the joints,
- gynecological disease of the mother, which can impede the child’s intrauterine movements - this could be uterine fibroids or adhesions in the pelvis,
- viral or bacterial infection in the first or second trimester of pregnancy,
- unbalanced diet: lack of vitamins B and E, phosphorus, iodine, calcium and iron.
Possible complications
Some complications arise already during osteotomy, others during the rehabilitation period.
- Incorrect fusion of bones. Occurs due to improper fixation of bone tissue fragments during surgery. With such a complication, repeated intervention is necessary.
- Non-union of bones. It may occur due to severe concomitant pathologies, smoking, impaired blood supply to the operated area, or osteoporosis. For treatment, a repeat operation is performed and special rehabilitation is prescribed.
- Compartment syndrome. Occurs if, during surgical manipulation, the muscles were strongly compressed by a tourniquet. For treatment, certain drugs are prescribed; if the case is severe, a fasciotomy is performed.
- Improper functioning of the joints located next to the surgical field. This complication is typical for the absence or violation of rehabilitation rules. Exercise therapy is prescribed.
- Infections. They can be introduced during surgery or due to improper wound care. An antibiotic is prescribed for treatment; in severe cases, revision surgery will be required.
- Nerve damage is a surgeon’s mistake or a peculiarity in the location of the patient’s nerve endings. The function of a damaged nerve cannot be restored.
- Thromboembolism. Occurs when anticoagulants are prescribed incorrectly, getting out of bed late, or the inability to wear compression stockings. To eliminate this complication, high doses of antiplatelet agents and anticoagulants are needed.
Treatment of pathologies of the cartilage of the hip joint in
Treatment of certain pathologies of articular cartilage in Israel can be carried out using conservative and surgical methods. Conservative treatment of such diseases involves:
- drug therapy;
- physiotherapy and massage;
- physical therapy;
- diet therapy;
- mud therapy, etc.
The basis of conservative treatment of hip joint cartilage is complex drug therapy. To get rid of debilitating pain, patients are prescribed analgesics, and if there are signs of an inflammatory process, non-steroidal anti-inflammatory drugs. In severe cases of inflammation, corticosteroids are indicated (including in the form of intra-articular injections).
Physiotherapy is one of the most important methods of conservative treatment of articular cartilage in Israel. Thus, electrophoresis allows you to enhance the effect of prescribed drugs. In addition, magnetic and laser therapy, UHF, ultrasound therapy, etc. can be prescribed.
To strengthen muscles, reduce swelling and pain, massage is prescribed. When massage is performed regularly by a competent specialist, it gives a pronounced positive result. To improve joint nutrition, it is recommended to regularly perform therapeutic exercises; such a set of exercises is compiled by a doctor. At the same time, it is not recommended to overload the joints.
Normalization of nutrition has a good effect. The patient is recommended to include in the diet foods that contain essential vitamins, minerals, and omega-3 fatty acids, which can have a positive effect on the condition of the hip joints. In addition, the diet helps you lose excess weight. All of these methods in combination make it possible to slow down the destruction of cartilage.
Treatment
Having discovered congenital dysplasia of the hip joint in the maternity hospital, they begin conservative treatment : first, wide swaddling is carried out, and from two to three weeks of age orthopedic pants are used.
In addition, parents are taught to perform hip abduction exercises before swaddling. After 3 months of life, they must undergo X-ray control, make sure that there is dysplasia, and put on Pavlik stirrups .
Their advantage is that they provide free access for the child’s hygiene, allow active movements of the legs with the hip and knee joints fixed at a 90° angle with the gradual achievement of full abduction of the hips.
Depending on the degree of dysplasia, Pavlik stirrups are worn for 3–6 months. The criterion for removing the stirrups is the complete restoration of the roof of the acetabulum, the angle of which in the Hilgenreiner diagram should be no more than 30°.
Why is hip abduction therapeutic?
Firstly , when the hip is abducted at an angle of 90°, the head is centered and constant pressure on the roof of the acetabulum is eliminated, which allows the elements of the hip joint to form correctly.
Secondly , constant irritation of the joint capsule and muscle functioning during active movements improves microcirculation, which also has a positive effect on the process of further development of the acetabulum.
| The goal of treatment of congenital dysplasia is to create optimal conditions for the development of the acetabular arch by the time the child reaches one year of age, that is, before the child begins to walk, normal biomechanical parameters must be restored in the joint. | |
Classification
Maternity deformities (cerebral palsy, brachial plexus, bone fractures, epiphysiolysis, etc.) usually occur as a result of injuries during assisted obstetric interventions.
Acquired orthopedic deformities are caused by various diseases of the support and movement apparatus: infectious, specific and nonspecific inflammations, tumors, degenerative-dystrophic processes, static disorders, consequences of injuries, etc.
However, many orthopedic deformities arise from a combination of different causes.
The proportion of congenital malformations of the apparatus of support and movement is very large. According to the World Health Organization, they occur 18 times in every 10,000 births. In addition, no trend towards a decrease in the number of birth defects is noticeable.
Progress of the operation
The instruments used are osteotomes (chisels) with a grooved or flat section, Gigli files, ultrasonic devices for cutting bones, and electric medical saws. After fragmentation of bones during osteotomy, their fixation is required, for which knitting needles, plates, screws or special devices are used. In some cases, plaster casts are additionally applied, but they try to avoid this so as not to cause discomfort to patients and eliminate the risk of developing joint contractures. Anesthesia - general anesthesia or local anesthesia, it all depends on the general health of the patient and the scope of the intervention.
Open osteotomy
A wide surgical field is created, the bone is exposed, the periosteum is separated and a dissection is made in the desired area. The fragments are connected with metal structures or a plaster cast is applied.
Closed method
The external incision on the skin is minimal - 2-3 cm. The muscle tissue is separated above the site of the intended bone dissection. The chisel is positioned longitudinally to cut the periosteum. After this, the instrument is turned perpendicular to the bone and cut through it with several blows with a hammer on the chisel. Nearby soft tissues, nerves and blood vessels are protected with special instruments to prevent damage.
Osteotomies are also classified according to their intended purpose: corrective (for example, for immobility of the knee joint), aimed at improving the supporting function, shortening the bone or lengthening it, derotational, etc.
If the patient has a clear bow of the big toe, a proximal corrective osteotomy is indicated. It is performed to correct the first metatarsal bone and is needed for the following symptoms:
- inability to put on shoes;
- pain syndrome;
- incorrect gait;
- bursitis.
Osteotomy of the upper and lower (planar) jaws can be performed on only one of the jaws or on both at the same time. It is indicated for developmental anomalies, serious problems with bite, existing negative consequences from previous operations, displacements, and fractures. Surgical intervention can be complete or fragmentary. As a result, after the operation, the process of biting and chewing food is easier for patients, the period of tooth wear is reduced, the risk of tooth decay due to poor bite is eliminated, the relationship between the jaws is normalized, which has a good effect on the appearance in general, and the risk of developing diseases of the temporomandibular joint is reduced.
Symptoms
When testing passive movements in the hip joint, the doctor bends the legs in the hip and knee joints to a right angle, and then slowly begins to spread them and feels that abduction on one side becomes limited (for unilateral dysplasia) or notes that abduction of both hips is limited (for bilateral dysplasia ).
Thus, hip dysplasia is characterized by three symptoms:
- the presence of additional folds on the medial surface of the upper third of the thigh;
- asymmetry of folds;
- limitation of hip abduction.
These are not pathogmonic symptoms, not absolute, but relative, indicating the presence of disorders in the hip joint, although they also occur in healthy children.
X-ray control
X-ray monitoring, which is carried out after three months of age, after the appearance of ossification nuclei of the epiphysis of the femoral head, makes it possible to clarify the diagnosis. The data obtained are assessed according to the Hilgenreiner scheme.
The following radiological symptoms are characteristic of congenital dysplasia: sloping roof of the acetabular fossa, flat, shallow acetabular fossa; late appearance of ossification nuclei of the epiphyses of the head; the head is centered without lateroposition.
Hilgenreiner scheme
On an x-ray of the pelvis and hip joints, a horizontal line is drawn through the V-shaped cartilages (Kaper's line).
The second line - a tangent line - is drawn from the upper edge of the roof of the acetabulum parallel to the latter and connected to the Köhler line. An angle is formed, which should normally be no more than 30°.
Next, along the horizontal Köhler line, segment d is laid from the center of the bottom of the acetabulum to the inner edge of the ossification nucleus. Normally, this segment is 1–1.5 cm.
An increase in the length of the segment indicates the presence of a lateroposition of the head. The next line is drawn from the top point of the roof in the form of a perpendicular to the Köhler line and continues to the thigh.
This perpendicular divides the acetabulum into 4 sectors. The ossification nucleus of the femoral head should always be in the lower internal sector.
In addition, a perpendicular is drawn from the Köhler line to the ossification nucleus of the femur. The length of this perpendicular is normally 1.5 cm. This indicator indicates the absence of upward (proximal) displacement of the head.
In addition, the absence of intra-articular displacement of the proximal end of the femur is indicated by Shenton’s line, which runs along the internal contour of the femoral neck and smoothly, without rupture, passes to the superomedial contour of the obturator foramen.
Characteristic features of capillary angiodysplasia
The International Association for the Study of Vascular Anomalies has introduced a classification of capillary malformations. The division criterion is the prevailing type of vessels. Accordingly, arterial, venous, lymphatic, capillary and mixed forms are distinguished.
The pathology is often confused with simple hemangiomas. However, clinically they have a number of differences. Capillary angiodysplasias are colored pink, bright red or purplish-blue, have uneven edges and do not protrude above the surface of the skin. They can be located on different parts of the body, including the face and limbs. Occupy a significant portion of the skin surface. In infancy, when you press on the spot, it changes color; in adulthood, this reaction of the capillaries disappears.
Capillary dysplasia is different from a vascular birthmark. The latter, as the child grows, gradually loses color and disappears, while the “wine stain” remains and can only increase in size. In addition, as the vessels grow and thicken, the spot begins to protrude above the surface of the skin, which is why it is often damaged and bleeds.
Prevention
Prevention of hip dysplasia consists in the high alertness of doctors regarding newborns in mothers with a high risk of developing hip dysplasia and parents regarding the risk of developing this pathology of the hip joints. The basis of prevention is a thorough repeated examination of newborn children and monitoring them during the first year of life, and if a pathology is detected, its treatment as early as possible. It is necessary to carry out educational work so that parents know how to identify hip dysplasia in children (characteristic symptoms).
The famous pediatrician Komarovsky believes that in the presence of initial degree joint dysplasia (unstable/immature hip), proper care for the child is necessary and, above all, wide swaddling (Fig. below). Wide swaddling for hip dysplasia in infants is mandatory for all babies at risk with signs of an immature joint.
Dr. Komarovsky, as an alternative, recommends (see the forum) to use disposable diapers 1-2 sizes larger than necessary (with a wide layer of sorbent between the child’s legs). In addition, all children diagnosed with “immaturity of the hip joint” should be classified as a risk group and be registered with a pediatric orthopedist with periodic ultrasonography of the hip joints. If the dynamics are negative, the doctor prescribes the wearing of specialized orthopedic structures.
In the future, children at risk are recommended to undergo a control X-ray examination of the hip joint 1-2 times a year. Also, for such children, physical activity is limited and attendance at special orthopedic groups is recommended.
Risks and dangers of performing an X-ray of the hip joint in a child
Before the onset of puberty, it is believed that radiography is indicated for the patient only in exceptional cases. In addition, an interval of at least 6 months must be observed between procedures. Prescribing hip x-rays in children more than twice a year is not recommended.
Contraindications for radiography for a baby are:
- immunodeficiency and other disorders of the immune system;
- predisposition to cancer;
- metabolic disorders;
- obvious atrophy of organs or muscles;
- diagnosed pathologies of the bone apparatus.
This diagnostic method may negatively affect:
- germ cells;
- bone marrow cells;
- eye lenses;
- epithelial cells that form the mucous membranes of organs and skin;
- organs of the endocrine system.
Despite this, the method of x-ray examination of joints in children is still used by doctors if necessary, as it is the most effective and objective of the existing ones. It is this that allows you to determine the presence of dislocation or dysplasia with an accuracy of up to 75%.
Hip dysplasia
This congenital pathology associated with improper development of the joint is quite common. According to statistics, up to 3% of newborns experience it. It occurs more often in girls than in boys. Disorders may be associated with underdevelopment or improper formation of the joint.
Depending on the location of the pathological process, three types of disease are distinguished:
- violation of the development of the acetabulum;
- upper bone dysplasia;
- violation of bone geometry (rotational dysplasia).
Pathology can develop on one or both joints. If a child develops unilateral dysplasia, it may manifest itself as asymmetry of skin folds. However, if the process affects both joints, the folds may be symmetrical. Therefore, this symptom alone is not enough to make a diagnosis.
More informative for the doctor is a sign of shortening of the femur. In this case, the baby’s knees in the supine position are located asymmetrically, which indicates congenital dislocation of the hip - a severe form of dysplasia.
Also, during the examination of newborns, the doctor checks joint mobility. In the absence of pathology, the baby’s legs are abducted to a position of 80-90°. In children with dysplasia, the angle does not exceed 50-60°.
Complications
In early childhood, the disease manifests itself as shortening of the hip, limitation or hypermobility of the joint. If left untreated, the weakness of the ligamentous apparatus increases, which leads to displacement of the femoral head, subluxation and dislocation. At an older age, children experience pain, limp when walking, and get tired quickly.
In adulthood, dysplastic arthrosis of the hip joint may develop. In girls, it may first appear during pregnancy. The disease manifests itself as pain, limited joint mobility, and deformation changes. Over time, the so-called vicious hip alignment develops, due to which the lower limb is in an anatomically incorrect position. This limits mobility and causes persistent pain. As the disease progresses, the patient is forced to resort to endoprosthetics.
Causes
Statistics show that a common cause of the disease is unfavorable heredity. Children with the pathology are more often born to parents who had a similar disease in childhood.
The second important reason is breech presentation of the fetus. It increases the likelihood of dysplasia 10 times. Also among the reasons, experts note oligohydramnios, high birth weight of the child, the mother taking certain medications during pregnancy, severe toxicosis, and unfavorable environmental conditions. The development of the musculoskeletal system of a newborn is negatively affected by tight swaddling.
Diagnostics
A pediatric orthopedic surgeon diagnoses hip dysplasia in children. If the pathology was detected immediately at birth, the doctor evaluates the clinical picture and draws up a treatment plan. In order to prevent undetected dysplasia, all newborns are subject to mandatory examination by a specialist during the first year of life. If the doctor detects signs of abnormal development of the hip joint, the baby is sent for examination.
The main diagnostic method is ultrasound diagnostics. At 2-3 months, the doctor may prescribe an x-ray. Until this time, such diagnostics are not used due to low information content. In newborns, most of the joint is formed by cartilage tissue, which is not visible on x-rays.
Treatment
If a child is diagnosed with dysplasia, the success of treatment depends on its timeliness. To fix the lower extremities in the anatomically correct position of abduction and flexion, special orthopedic devices are used. They vary in design and rigidity. As a rule, products are used that fix the joint, but at the same time maintain mobility of the lower extremities.
In addition to wearing bandages and splints, special exercises and massage are recommended for joint dysplasia. In case of congenital dislocation, children aged 2 to 5 years undergo a one-stage closed reduction and a plaster is applied to limit the mobility of the joint in order to fix it in the correct position. In severe cases, surgical treatment may be required.
What is dysplasia and why diagnose its presence?
Out of one hundred newborn children, three are born with dysplasia of the joint joints. A feature of the infant’s musculoskeletal system is the presence of more cartilage tissue than bone. The baby's bones do not yet contain a sufficient amount of calcium; they are more flexible than those of adults. Therefore, children’s fractures are not the most common phenomenon, while dislocations and subluxations are much more common among them.
Dysplasia is a congenital disorder of the anatomical structure and development of the hip joint. Pathology can cause impaired mobility and chronic hip dislocation. Doctors do not yet have accurate information about what exactly causes it to appear. It is believed that the disorder develops in the fetus at 2-3 months of pregnancy. This may be due to past infectious diseases, unfavorable environmental conditions, exposure to toxins and bad habits, such as drinking alcohol or smoking.
Another theory suggests that the formation of chronic subluxation of the hip joint is facilitated by excessive accumulation of oxytocin, a pregnancy hormone that triggers the onset of labor. It is produced in the body of the expectant mother by the third trimester of pregnancy, and causes an increase in muscle tone in the fetus, which is why dysplasia develops.
The appearance of such a diagnosis is especially facilitated by the presence of the fetus in the womb with its legs crossed.
The risk of developing pathology increases the incorrect position of the fetus in the womb, as well as the factor of hereditary predisposition.
In some children born with dysplasia of the TJ joint, its reduction occurs arbitrarily immediately after birth.
In essence, dysplasia is a discrepancy between the articular surfaces. If the child lies with his legs crossed, the acetabulum and the surface of the femoral head are not in direct contact during development. Even normally, the joints and bones of the fetus are not particularly stable - this is due to the need to facilitate its passage during childbirth. However, with dysplasia, the development of joint ossification points occurs late, and the ossification nuclei are smaller in size than normal. Their vertical-lateral displacement relative to the normal position is clearly visible visually. Dysplasia is also characterized by a slowdown in the ossification process.
Types and degrees of dysplasia
- improper development of the acetabulum, it partially loses its spherical shape and becomes flatter and smaller in size;
- underdevelopment of the cartilaginous rim that surrounds the acetabulum;
- weakness of the hip ligaments.
- Degrees of hip dysplasia
- Actually dysplasia. There is abnormal development and inferiority of the hip joint. But its configuration has not yet been changed. In this case, it is difficult to identify pathology during examination of the child; this can only be done with the help of additional diagnostic methods. Previously, this degree of dysplasia was not considered a disease; it was not diagnosed or prescribed treatment. Today such a diagnosis exists. Overdiagnosis occurs relatively often when doctors “identify” dysplasia in a healthy child.
- Pre-dislocation. The hip joint capsule is stretched. The head of the femur is slightly displaced, but it easily “falls” back into place. Subsequently, preluxation transforms into subluxation and dislocation.
- Subluxation of the hip. The head of the hip joint is partially displaced relative to the socket. It bends the cartilaginous rim of the acetabulum and moves it upward. The femoral head ligament (see above) becomes tight and stretched
- Hip dislocation. In this case, the head of the femur is completely displaced relative to the acetabulum. It is located outside the cavity, above and outward. The upper edge of the cartilaginous rim of the acetabulum is pressed by the head of the femur and bent into the joint. The joint capsule and ligament of the femoral head are stretched and tense.
Types of hip dysplasia
- Acetabular dysplasia. A pathology that is associated with impaired development of only the acetabulum. It is flatter and reduced in size. The cartilaginous rim is underdeveloped.
- Femoral dysplasia. Normally, the femoral neck articulates with the body at a certain angle. Violation of this angle (decrease - coxa vara or increase - coxa valga) is a mechanism for the development of hip dysplasia.
- Rotational dysplasia. Associated with a violation of the configuration of anatomical formations in the horizontal plane. Normally, the axes around which all joints of the lower limb move do not coincide. If the mismatch of the axes goes beyond the normal value, then the position of the femoral head in relation to the acetabulum is disrupted.
Stages of joint dysplasia
Depending on how susceptible the articular apparatus and its parts are to pathology, the following stages of dysplasia are distinguished:
- preluxation: the mildest degree, when the head of the femoral bone can move inside the acetabulum, and the joint itself is characterized by instability;
- subluxation: the stage when anatomical and morphological changes begin to form, the head of the femur moves away from the glenoid cavity, but remains within the limbus (a cartilaginous plate that prevents the head from moving upward);
- dislocation: in this case, the head of the femur completely comes out of the socket of the joint, while the limbus moves upward, and the ligaments of the joint are stretched.